- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
25 year old woman with Brain AVM (arteriovenous malformation)
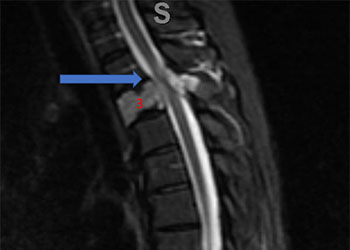
Spinal Embolization Treats Aggressive Comprehensive T3 Verterbral Body Hemangioma
October 26, 2021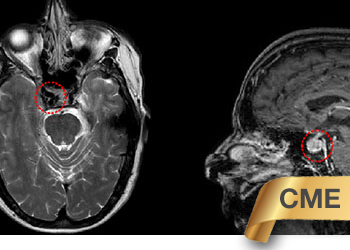
Direct Carotid Cavernous Fistula (CCF)
October 26, 2021Examination:
Her general and neurological examinations were normal. She was alert and oriented. Her cranial nerves were intact and her motor and sensory examinations were normal. Her vitals were normal other than a mild tachycardia (105) and her labs were normal.
Imaging:
Head CT was consistent with a small acute left intraventricular hemorrhage (Figure 1).
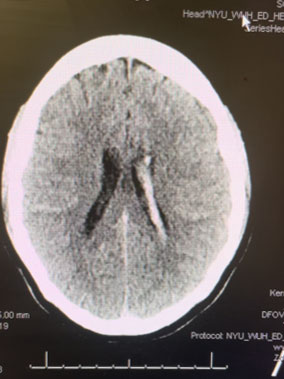
Fig. 1
MRI was consistent with a left deep frontal AVM (Figure 2).
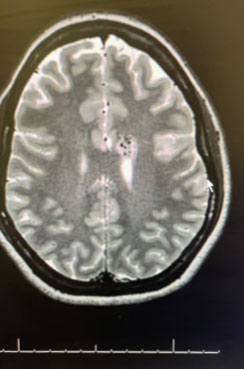
Fig. 2
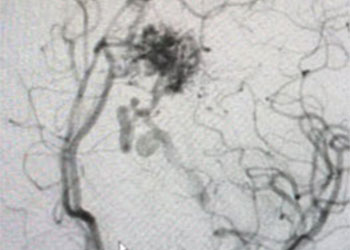
Angiogram (Figure 3 and 4) confirmed the presence of a deep left frontal AVM without any associated aneurysms.
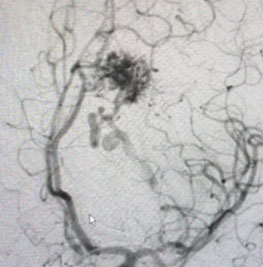
Fig. 3
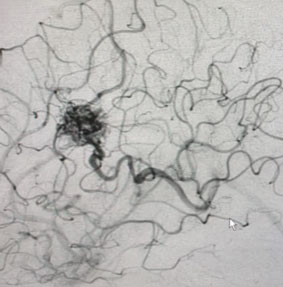
Fig. 4
Hospital Course:
The patient was observed for several days in the ICU. Her exam remained normal and follow up Head CT’s showed no change and no development of hydrocephalus.
Treatment:
Several weeks after the hemorrhage, the patient was brought for definitive treatment of her Brain AVM with Gamma Knife. On the day of the procedure, she underwent Brain MRI and angiogram to localize the AVM nidus. A plan was made to treat the nidus with 24Gy to the 50% isodose line (Figure 5). The 50% isodose line was created to be very tight to the AVM nidus and encompassed a volume of 1.3 cubic cm. The patient tolerated the procedure well and was discharged the same day.

Fig. 5
Brain AVM’s are usually thought to be congenital anomalies. They bleed at a rate of about 3-4% per year, with about half of those leading to serious disability or death. About 7% of Brain AVM’s have associated brain aneurysms, which can often resolve after the AVM is treated. Very small AVM’s can sometimes be treated with neuro-endovascular embolization alone. Giant AVM’s may not have any surgical options. Small superficial AVM’s in non-eloquent areas that have bled, can be considered for surgical removal after neuro-endovascular embolization. For most patients with Brain AVM’s, one day, outpatient Gamma Knife treatment, is an excellent option, and we would consider the treatment of choice. This patient had a small deep AVM that had bled, in the dominant hemisphere, and near the motor region. This AVM will likely disappear over the next 1-2 years.
CATEGORY: BRAIN // 25 YEAR OLD WOMAN WITH BRAIN AVM (ARTERIOVENOUS MALFORMATION)
25 year old woman with Brain AVM (arteriovenous malformation)
Chief Complaint:
This is a 25-year-old woman who came to the hospital with the chief complaint of new headache, nausea, and vomiting.
History of Present Illness:
The headache had begun suddenly just hours earlier. She had had no such prior headaches. The headache was in the posterior head and neck region. She also noted paresthesias in her arms. Her history was noteworthy only for asthma.