- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Personality and Behavioral Changes Resulting from an Anterior Skull Base Tumor
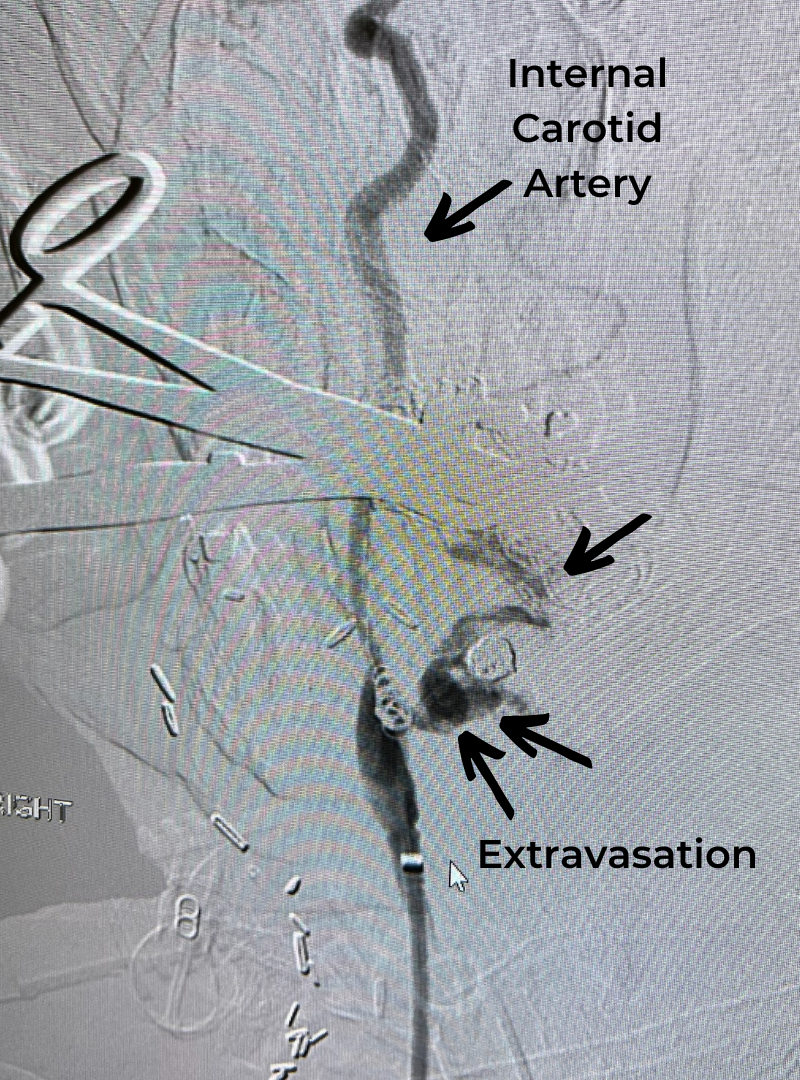
Carotid Blowout Requires Life-Saving Intervention
June 16, 2022
Endarterectomy Treats Symptomatic Carotid Stenosis
July 1, 2022This is a 49-year-old otherwise healthy female who presented with bifrontal and retro-orbital headaches, behavioral changes, and forgetfulness. Symptoms have been progressively worsening over the past month. Her neurologic exam revealed a pronator drift, otherwise was unremarkable. MRI brain demonstrated a large extra-axial homogeneously enhancing mass of the anterior cranial fossa, resulting in significant mass effect and vasogenic edema (Figure 1a and 2a). Imaging was most consistent with a planum sphenoidale meningioma. She was referred to Dr. Xavier Gaudin for neurosurgical evaluation.
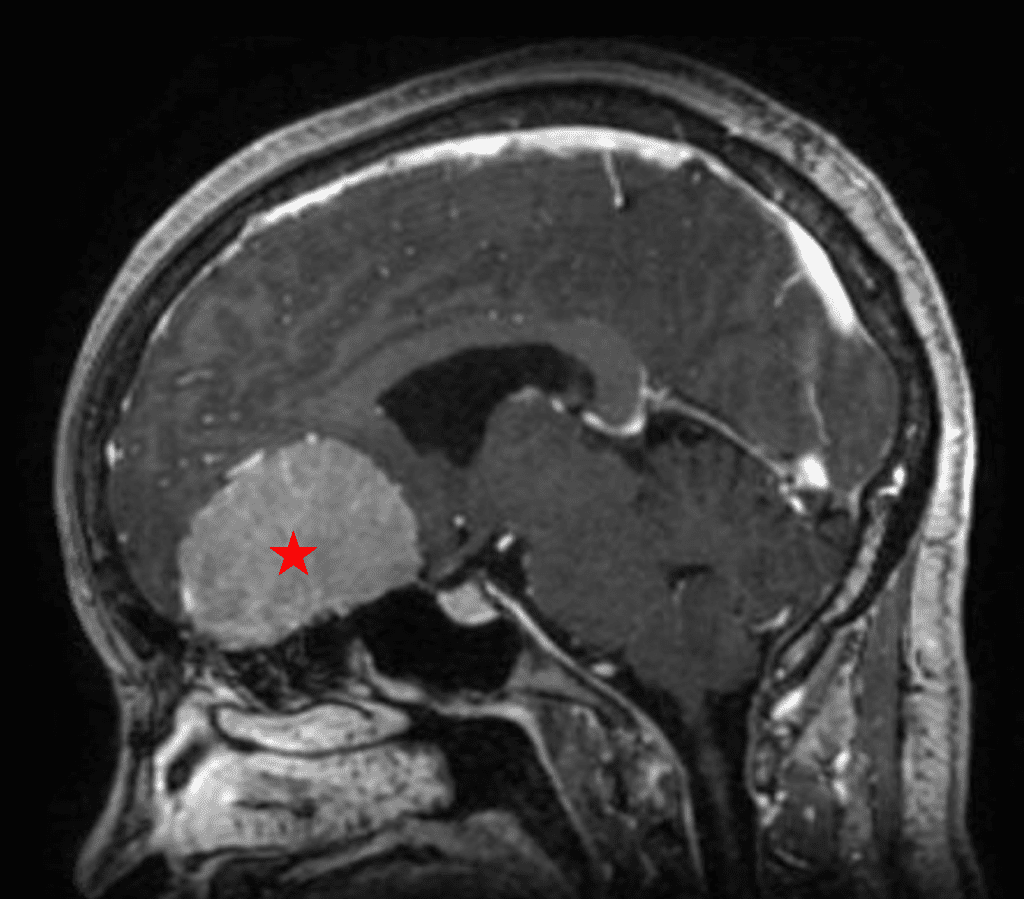
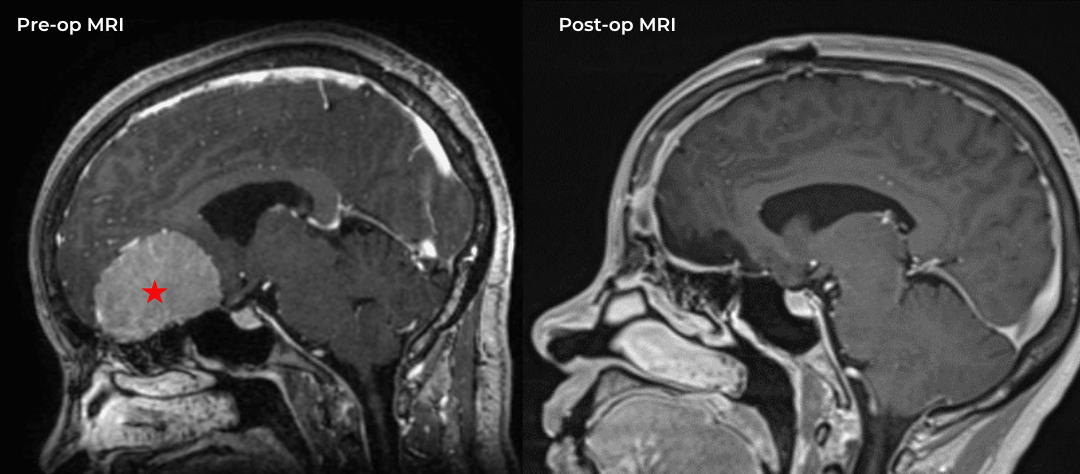
Figure 1a – Preoperative MRI demonstrating an extra-axial enhancing mass of the anterior cranial fossa.
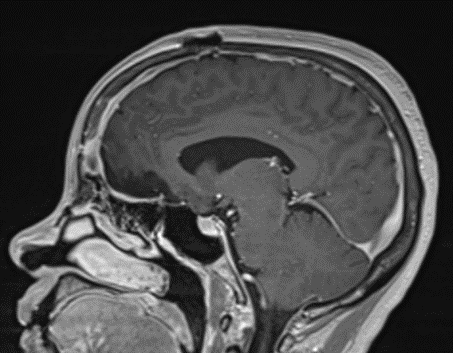
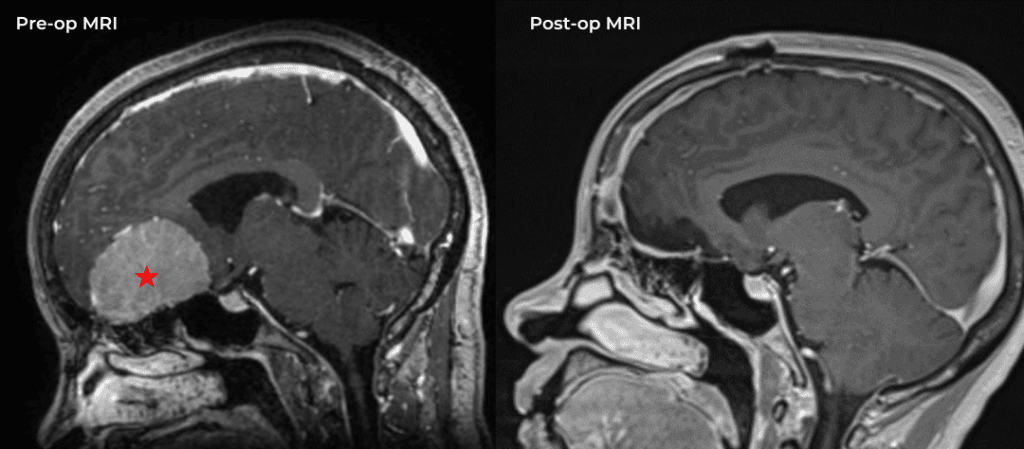
Figure 1b – Postoperative MRI demonstrating a complete resection without residual enhancement.
She was started on high-dose steroid and antiseizure prophylactic medicine. Surgical intervention was offered for mass effect, symptomatic relief, neurologic preservation, and histopathologic diagnosis. Dr. Gaudin performed a bifrontal craniotomy with complete resection of neoplasm through an interhemispheric and subfrontal approach. Postoperative imaging demonstrated a gross total resection without residual tumor and resolution of mass effect (Figure 1b and 2b). Intraoperative pathology was consistent with meningioma, WHO grade 1. She recovered very well, and was discharged home on postoperative day 3. On her follow-up outpatient visit, her preoperative symptoms had fully resolved, and her olfactory sense was maintained.
Midline anterior cranial fossa meningiomas are rare, and classified according to their anatomical site of origin. This includes the olfactory groove, planum sphenoidale, and tuberculum sella. Although they are benign and slow growing, they can invade the skull base and ethmoid sinus. Primary blood supply is usually from the anterior and posterior ethmoidal arteries. They are most often found in women, in their 5th and 6th decades of life. They commonly present with cognitive impairment and behavioral changes, which can be mistaken for early onset dementia or depression. Headaches, visual changes, and anosmia may also be present. Surgical resection generally reverses the cognitive and behavioral changes, and can be curative if gross total resection is attained.
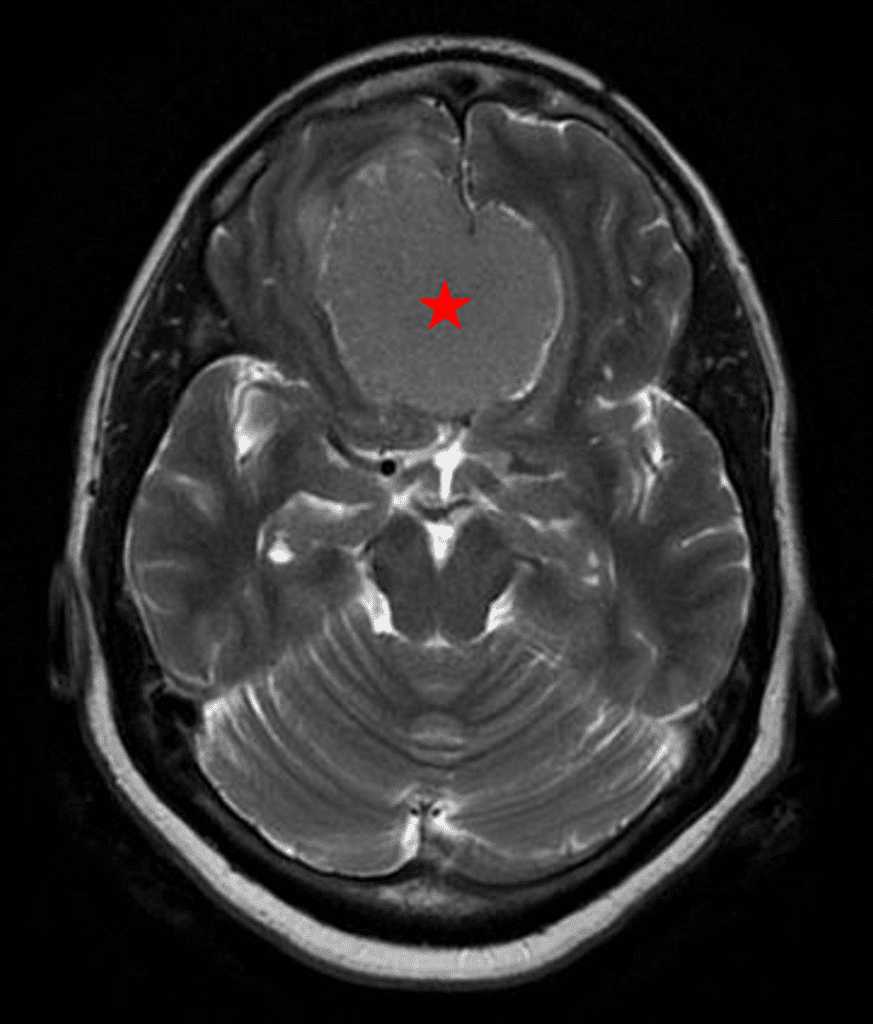
Figure 2a – Preoperative MRI demonstrating an extra-axial lesion with surrounding vasogenic edema and mass effect on the frontal lobes.
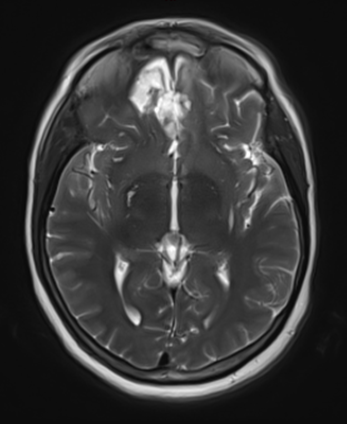
Figure 2b – Postoperative MRI demonstrating resolution of mass effect.
References:
Zygourakis, Corinna C et al. “Management of planum/olfactory meningiomas: predicting symptoms and postoperative complications.” World neurosurgery vol. 82,6 (2014): 1216-23. doi:10.1016/j.wneu.2014.08.007
Farrow, Megan. “Planum Sphenoidale Meningioma Symptoms Mimic Those of Early-Onset Dementia.” Radiologic technology vol. 92,4 (2021): 408-410.
DeMonte, Franco, and Shaan M Raza. “Olfactory groove and planum meningiomas.” Handbook of clinical neurology vol. 170 (2020): 3-12. doi:10.1016/B978-0-12-822198-3.00023-9
CATEGORY: BRAIN // PERSONALITY AND BEHAVIORAL CHANGES RESULTING FROM AN ANTERIOR SKULL BASE TUMOR
Personality and Behavioral Changes Resulting from an Anterior Skull Base Tumor
Authors
To learn more about the author, click his name or photo: