- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Cerebral Metastases from Non-Small Cell Lung Cancer
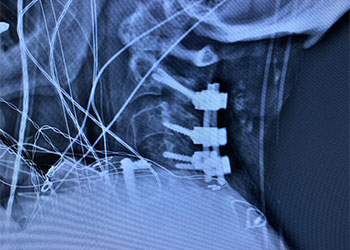
Cervical Laminectomy and Fusion
October 27, 2021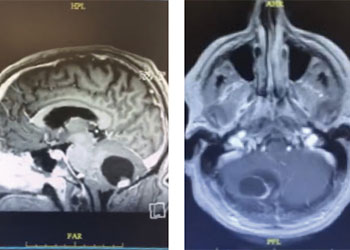
Cerebellar Hemangioblastoma
October 27, 2021Surgical resection was felt to be most appropriate given the extensive size not being amenable to radiation, degree of symptomatic mass effect, favorable accessibility and non-eloquent location, and histopathologic diagnosis. He underwent a right frontal craniotomy, performed by Dr. Xavier Gaudin, with a three-quarter bicoronal flap for resection of both the sub frontal and superior subcortical masses. Grossly, the masses appeared so, friable, purple, and gray in appearance with a disncve plane from the parenchyma. Pathology was consistent with poorly differentiated adenocarcinoma from lung origin.
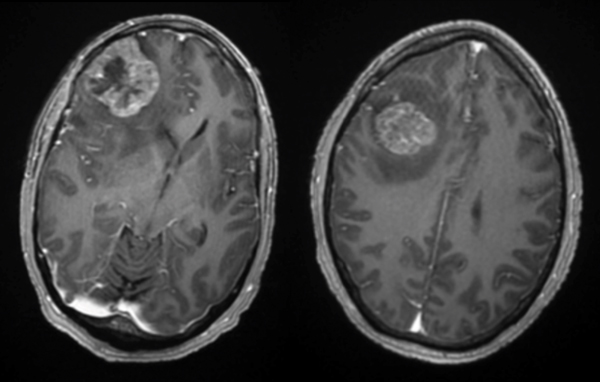
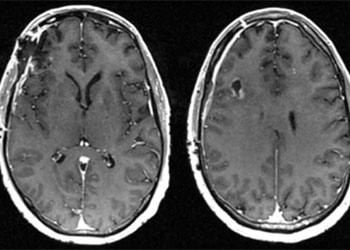
Pre-op
Post-op
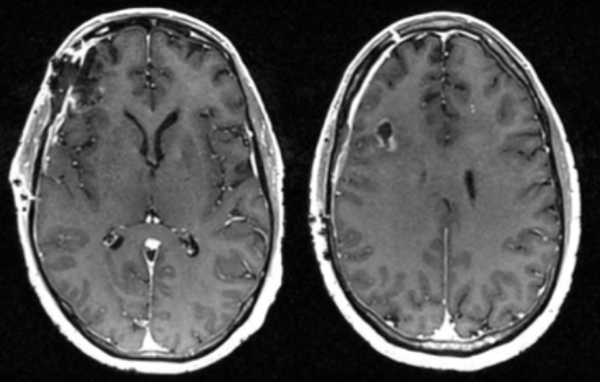
Follow up imaging demonstrated a gross total resection for both intracranial metastases. The patient tolerated the surgery well and was discharged home on postoperative day four. At one-month follow-up, he was neurologically back to his baseline with a resolution of previous headaches and behavioral changes. He underwent postoperative stereotactic radiosurgery (Gamma Knife) to each surgical bed, followed by chemotherapy.
CATEGORY: BRAIN // CEREBRAL METASTASES FROM NON-SMALL CELL LUNG CANCER
Cerebral Metastases from Non-Small Cell Lung Cancer
This is a 56-year-old man with a history of COPD and asthma who presented with a syncopal event and one week of retro-orbital headaches, blurry vision, and personality changes including apathy and disinhibition. He had a 40- pack-year smoking history but no prior malignancy. The exam revealed a pronator dri on the le upper extremity. MRI brain demonstrated 2 large right frontal heterogeneously enhancing masses with vasogenic edema causing midline shi and subfalcine herniation. The largest lesion was 3.9 x 4.0 cm on the inferior/sub frontal cortical surface, while the other was 3.0 x 2.7 cm in the superior subcortical frontal lobe. Further imaging showed a mediastinal mass suspicious for malignancy. He was started on Decadron for edema and Keppra for seizure prophylaxis.
Authors
To learn more about the author, click his name or photo:

