- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Cervical Fusion Corrects Next Segment Degeneration
Pineal Region Meningioma
February 2, 2022
Indirect EDAS Revascularization Treats Moya-Moya Syndrome
February 18, 2022Patient is a 60-year-old female who presents with severe right upper extremity pain and weakness over several months.
She had a prior C6-7 ACDF with plate and subsequently developed next segment degeneration at C5-6 which resulted in a second ACDF at C5-6 with removal of the prior C6-7 plate.
Current imaging studies (Figs. 1 and 2) demonstrated significant degenerative collapse of C45 segment, retrolisthesis and with severe right foraminal stenosis as well as C3-4 degenerative disc degeneration with moderate compression of thecal sac. Patient failed conservative management and it was decided, given her prior two anterior procedures, that an excellent decompression could be accomplished with a posterior laminectomy, foraminotomy and fusion to maintain alignment.
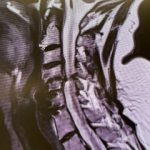
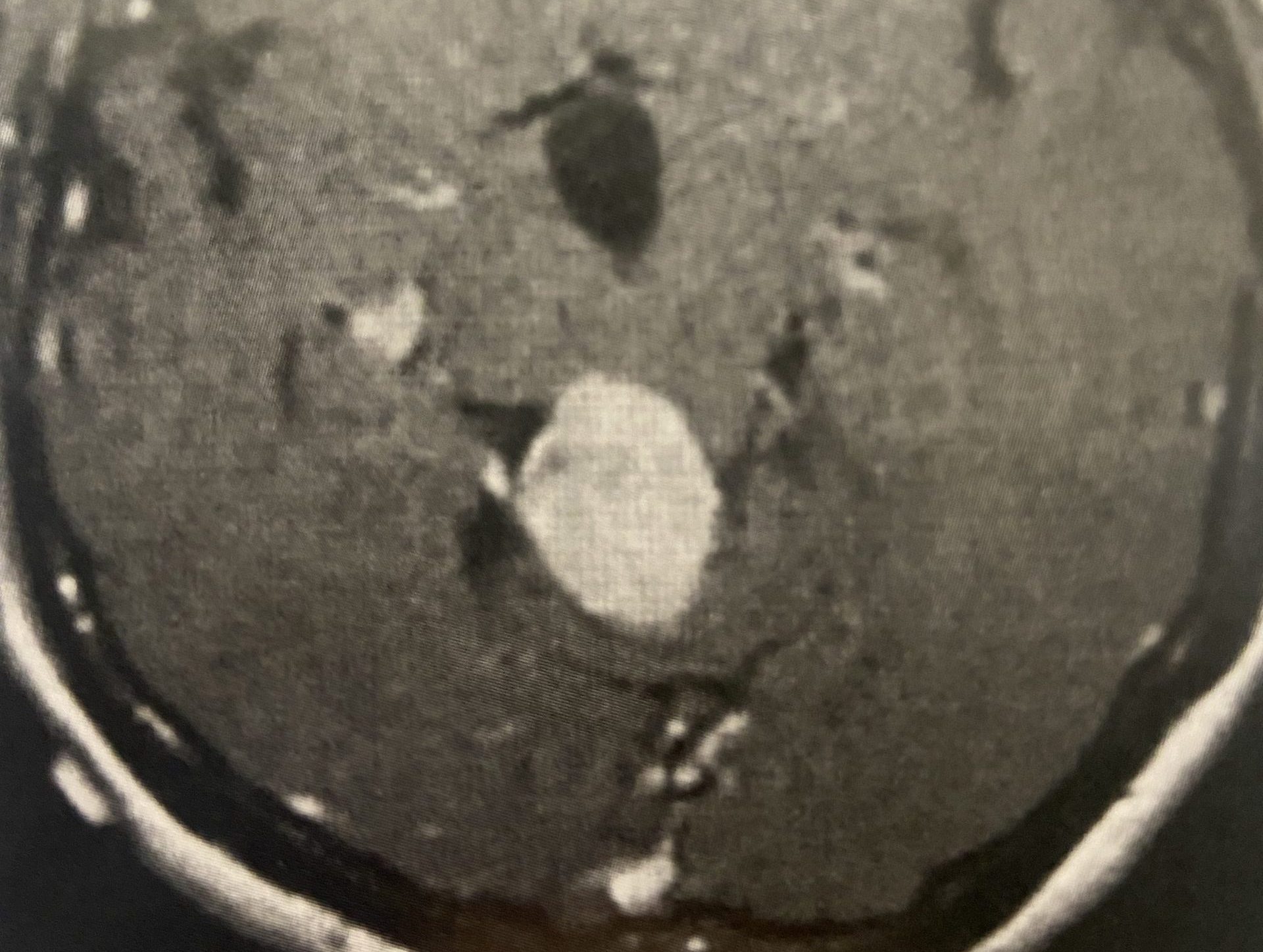
(Fig. 1) Sagittal T2 cervical MRI demonstrates significant C34 and C45 disc degeneration and osteophyte formation and instability status post anterior cervical discectomy and fusion C5-C7.
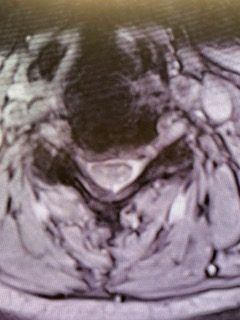
(Fig. 2) Axial T2 cervical MRI at C4-5 demonstrating significant osteophytic disease with bilateral neural foraminal compression of the C5 nerve roots, right greater than left.
A C2 to C6 posterior cervical laminectomy was conducted as well as a C3-C6 fusion with instrumentation. Most importantly an extensive foraminotomy was performed of the right C5 nerve root, which was followed laterally with a Kerrison punch.
Anteriorly to the C45 facet joint the right C5 nerve root was found in a more superior position under the C4 inferior process. The method of a posterior foraminotomy allowed an extensive decompression of the nerve root which would not have been as well accomplished with an anterior approach.
Given the prior two anterior surgeries, the patient had a reasonable lordosis, and the primary pathology was foraminal stenosis, it was of our opinion that a posterior approach was a better choice than an anterior approach.
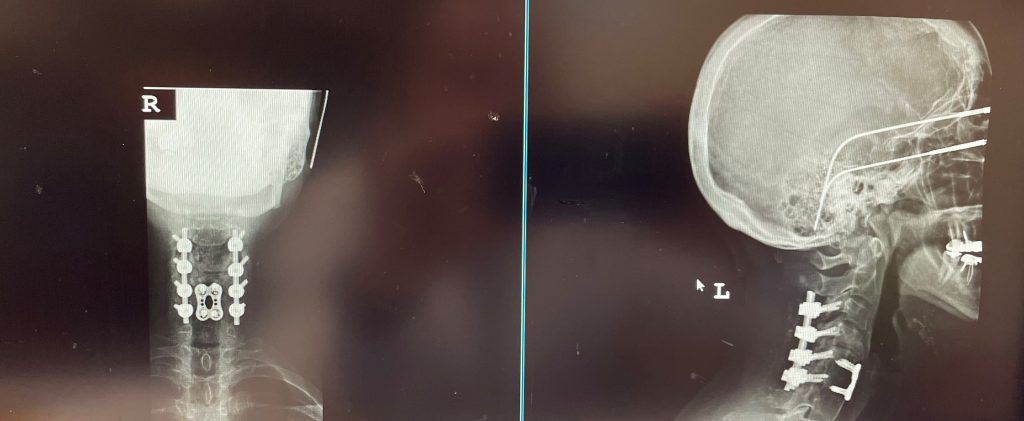
(Fig. 3) AP and Lateral cervical X-ray 6 months from surgery demonstrates a stable construct and alignment.
Postoperatively the patient had an uneventful course with relief of her right arm pain and stable construct (Fig. 3) at follow up at 6 months.
Key Learning Points:
- Patients with next segment degeneration from prior cervical fusion surgery is a fairly common phenomenon.
- In a meta-analysis, Kong et al reported in one study a 2.9 percent per year development of symptomatic adjacent level disease after single-level anterior cervical discectomy and fusion and estimated that about 25.6% of patients would have symptomatic adjacent level disease within 10 years after their index surgery. This can be in the form of disc degeneration with collapse, ligamentous and facet hypertrophy, retrolisthesis or spondylolisthesis, or herniated disc that results in nerve root or spinal cord compression.
- In the cervical spine patients with symptomatic neural foraminal or spinal canal stenosis can present with severe radicular pain, numbness, and weakness.
- Patients with spinal cord compression can present with symptoms and signs of myelopathy. This can consist of weakness in the triceps and finger extensors as well as hip flexors and dorsiflexors with or without pathological reflexes. The patients can also present with numbness and tingling of their hands and difficulty with fine movements like buttoning a shirt.
- A posterior approach to decompress the spinal cord or individual nerve roots is best performed when the patients have a reasonable lordosis. This is a biomechanical issue. With a kyphotic cervical spine, a posterior decompression would further enhance the anterior compression and deformity which would decrease the effectiveness of the decompression.
- In this case, the patient has had two prior anterior cervical discectomies and fusions with a good lordosis. It was felt to be a better option to approach the decompression posteriorly as a third anterior approach would involve significant scarring with a higher risk of complications such as vocal cord palsy and swallowing difficulty. Because of the prior anterior fusion, we felt it was necessary to perform an extension of the fusion to C3 to prevent the development of further instability and maintenance of decompression. There is a fulcrum-effect above the prior anterior fusion.
- With posterior decompression the signal for development of compensatory spondylotic disease with resultant development of spinal stenosis and/or nerve root compression remains if it is not augmented by posterior fusion.
References:
Kong, L, Cao, Jumming, Wang, Lingeng et al (2016). Prevalence of adjacent segment disease following cervical spine surgery: A PRISMA-compliant systematic review and meta-analysis. Medicine, 95(27), e4171. Doi: 10.1097.
CATEGORY: SPINE // CERVICAL FUSION CORRECTS NEXT SEGMENT DEGENERATION
Cervical Fusion Corrects Next Segment Degeneration



