- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Endarterectomy Treats Symptomatic Carotid Stenosis
Personality and Behavioral Changes Resulting from an Anterior Skull Base Tumor
June 27, 2022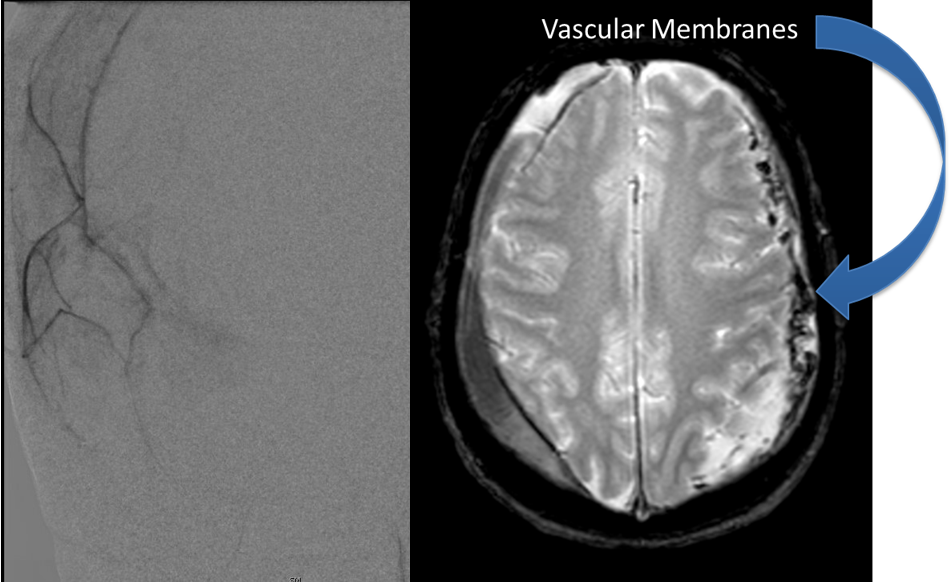
Middle Meningeal Artery Embolization of Bilateral Subacute Subdural Hematomas
July 22, 2022
Fig. 1 – Pre-operative imaging using a diffusion-weighted image sequence, shows multiple areas of most likely embolic stroke in the right frontal white matter.
Fig. 2 – Pre-operative imaging shows multiple areas of most likely embolic stroke in the right corona radiata.
The patient is an 83-year-old man who has a history of hypertension and prior strokes who presented with a brief episode of left arm greater than leg weakness that resolved. He also had some slurred speech that also resolved.
MRI imaging using the diffusion-weighted image sequence, which is highly sensitive for acute stroke showed multiple areas of most likely embolic stroke in the right frontal white matter (Figure 1) as well as the right corona radiata (Figure 2).
He was studied with noninvasive imaging most significantly, which was a CTA that confirmed a high-grade carotid stenosis from a calcified atherosclerotic plaque. This is seen in Figure 3 which is a coronal CTA. The patient was evaluated for carotid revascularization, and given the high-grade critical stenosis detected on the CTA and the carotid duplex, he was a good candidate, given the high-stroke risk of the lesion if left untreated.
Fig. 3 – Pre-operative CTA image confirms high-grade carotid stenosis from a calcified atherosclerotic plaque.
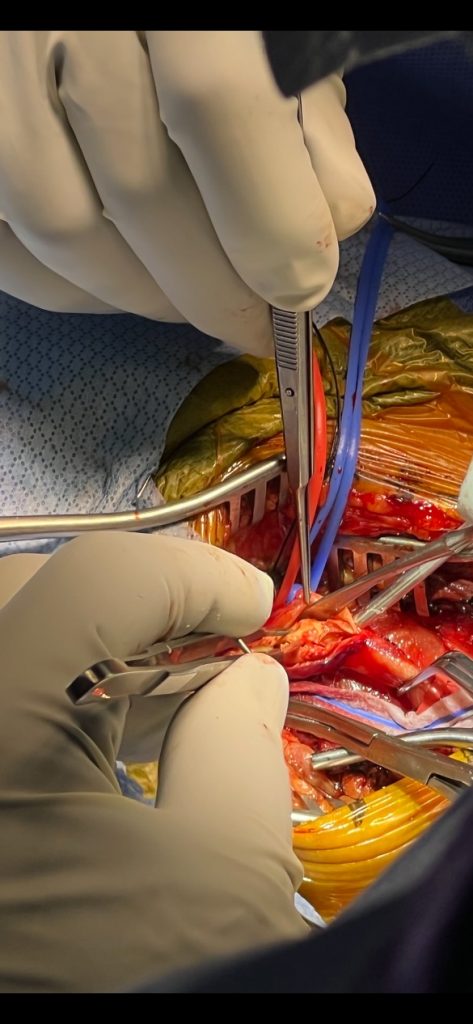
Fig. 4 – Image of the common carotid mobilized external and internal carotid arteries.
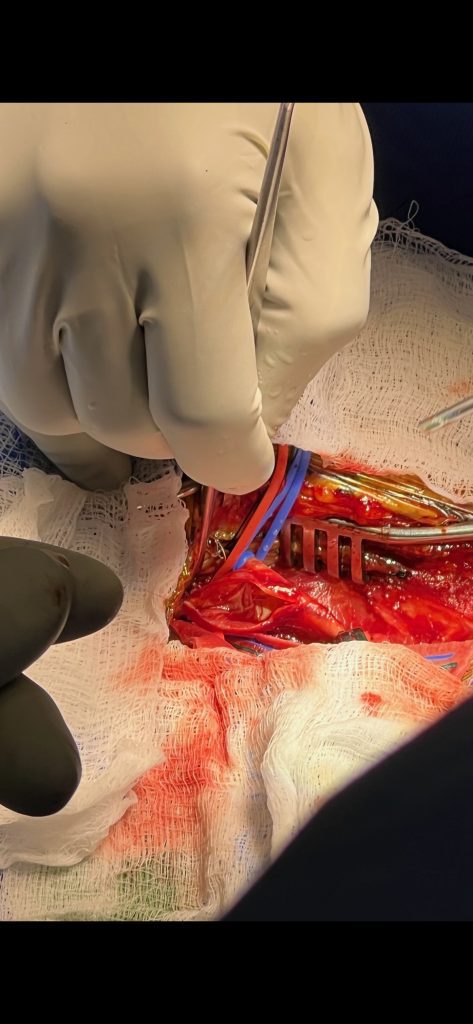
Fig. 5 – Image of the vessel after removal of the plaque.

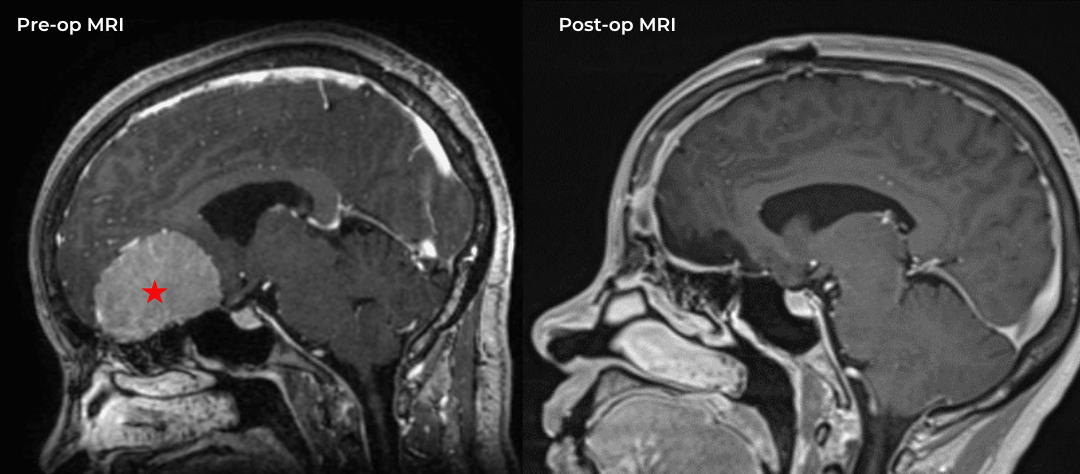
Fig. 6 – Doppler confirms patency of all vessels after closure.
After a discussion with the patient about the risks and possible benefits of revascularization, specifically carotid endarterectomy, the patient agreed, and we proceeded to perform a right carotid endarterectomy with neurophysiologic monitoring. The common carotid external and internal carotid were all identified and then dissected out cleanly and vascular loops placed around them. The common carotid artery was then incised into plaque and the arteriotomy was carried into the internal carotid artery beyond the plaque, and then the plaque shelled out as seen in Figure 4. Once the entire plaque is removed (Figure 5), the inside of the vessel is cleaned out of all remaining debris, prior to closure.
Once the artery is completely closed, and all the clamps are removed, the Doppler confirms good flow, as seen in Figure 6.
DISCUSSION:
- Symptomatic severe carotid stenosis as is seen in this gentleman from atherosclerotic plaque at the carotid bifurcation is a well-described and well-known clinical entity.
- Multiple large, randomized trials have shown the safety and efficacy of carotid endarterectomy to markedly reduce the stroke risk if performed successfully without complication by a skilled surgeon.
- Carotid stenting is another option that is always discussed with patients, but one that I typically reserve for high-risk patients, of which this patient was not.
CATEGORY: ENDOVASCULAR // ENDARTERECTOMY TREATS SYMPTOMATIC CAROTID STENOSIS
Endarterectomy Treats Symptomatic Carotid Stenosis