- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Patient with Cervical Spine Trauma Suffers Multiple Concurrent Pathologies
Posterior Fossa Brain AVM – 20-Year Follow-Up
March 21, 2022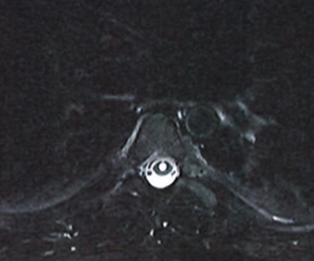
Severe Intractable Postural Headaches in a Young Lady
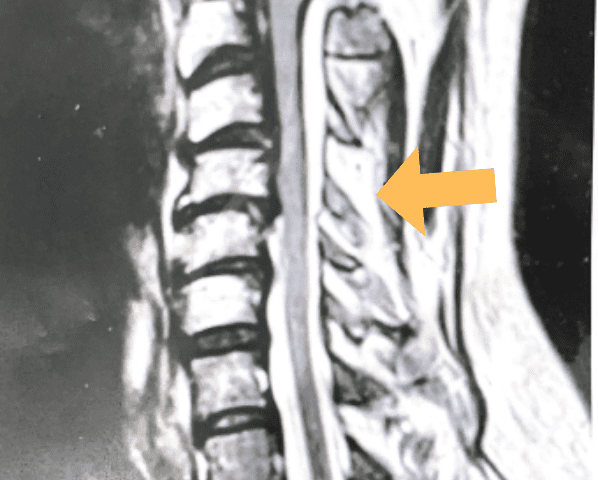
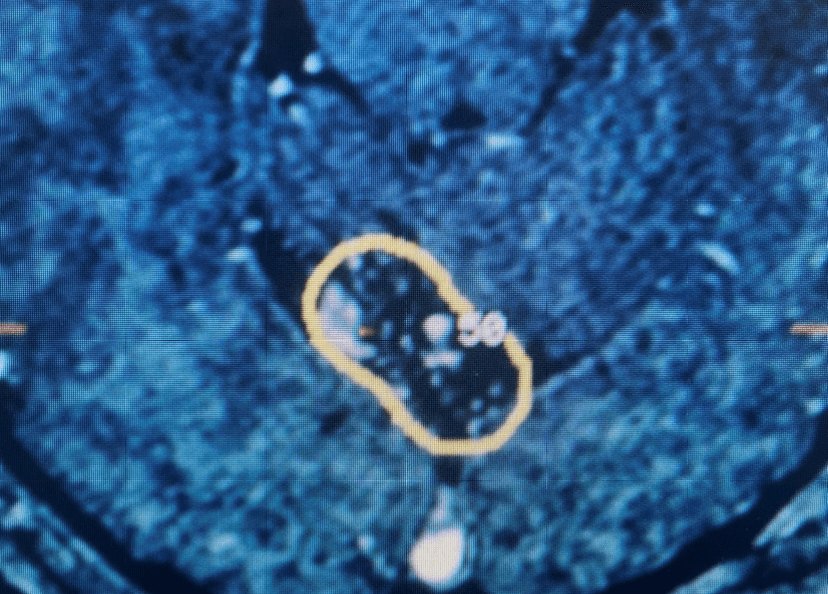
April 1, 2022This 57 year-old male presents with severe neck, left shoulder and arm pain and weakness in his hand since being involved in a motor vehicle accident nine months prior. The patient had subsequent left shoulder surgery although he still complained of pain postoperatively and his weakness persisted. He was on no blood thinners. He underwent imaging. The cervical spine MRI revealed an extensive dorsal epidural collection from C1-2 through C5 with associated spinal cord compression. In addition there were multisegmental degenerative changes with foraminal stenosis worse at C4-5 (Fig. 1a and 1b).
(1a) Sagittal and axial T2-weighted cervical MRI demonstrating extensive dorsal epidural collection with hyperintense signal consistent with fluid causing spinal cord compression.

(1b) Hyperintense signal (arrow) at the C3-4 interspinous space consistent with ruptured interspinous ligament,C4-5 (Fig. 1a and 1b).

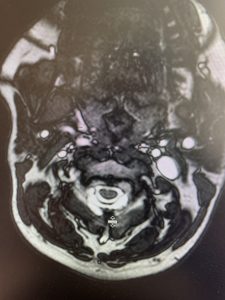
(2a) Lateral Flexion cervical x-rays demonstrating 8mm of splaying of the C34 interspinous distance

(2b) Lateral Flexion cervical x-rays extension image demonstrating 8mm of splaying of the C34 interspinous distance.
The fluid was possibly consistent with CSF versus chronic hematoma. The patient was also noted to have a high signal within the interspinous space of C3-C4. This high signal was consistent with a ruptured C3-4 interspinous ligament. Cervical flexion-extension x-rays demonstrated 6 mm of widening of the C3-4 interspinous space on flexion x-ray consistent with cervical instability (Fig. 2a and 2b).
It was felt that the patient was unstable and the patient had signs of early cervical myelopathy secondary to spinal cord compression. The patient consented to undergo exploration and evacuation of the collection and to decompress and stabilize the cervical spine. Upon laminectomy we noticed a ruptured C3-4 interspinous ligament that was consistent with the preoperative imaging studies. After revealing the epidural space during the laminectomy, a large dorsal membrane or pseudomeningocele was noted above a clear fluid collection that was posterior to the dura that was compressing the spinal cord. This membrane was fenestrated and we evacuated the collection which was consistent with CSF. Also during the course of the laminectomy we noted that the source of the CSF leak to be on the left at the takeoff of the C4 nerve root for which the dural sleeve was “degloved” but the fascicles were intact. We repaired with muscle and dural sealants. We completed a C2-C7 laminectomy. The patient had an additional fusion C3-C6 with segmental instrumentation to prevent kyphotic deformity.
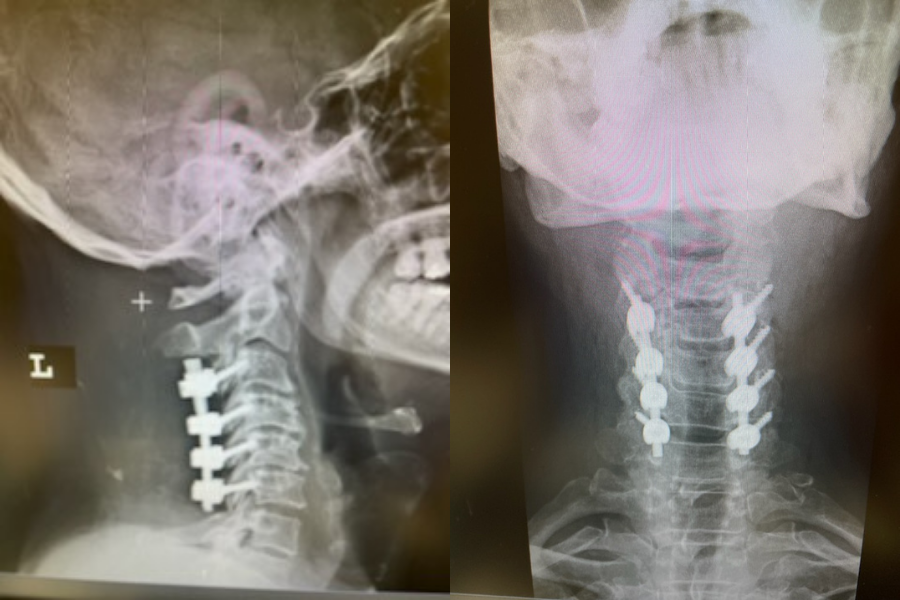
(3) Post operative AP and lateral cervical x-ray demonstrating good placement of hardware and alignment.
Patient did well from surgery with reduced pain in left shoulder and no further leak.(Fig. 3)
Key Learning Points:
This case illustrates several problems: Patients with traumatic cervical spine injuries can suffer multiple concurrent pathologies. This can be a result of underlying degenerative disease with acute secondary compression of the spinal cord and resultant acute clinical myelopathy. They may also develop as a result of their acute traumatic process instability or, as a result of the change in biomechanics, the potential to develop chronic instability. Also, as a result of the acute trauma these patients may develop secondary cervical epidural collections such as a hematoma or CSF which can compress the spinal cord.
This patient had an interspinous ligament rupture which could cause potential glacial instability and a kyphosis which could result in secondary degenerative compensatory changes. The interspinous ligament acts as a posterior tension band in extremes of flexion, therefore preventing kyphosis. High velocity injuries such as motor vehicle accidents are well documented to result in cervical nerve root avulsions. These nerve root injuries which can be multiple are traction injuries and may be associated with a tear in the meninges through the vertebral foramina and result in CSF collections and pseudomeningocele. The fact that the patient had distal weakness may be a result of spinal cord compression. The left C4 nerve root injury could have resulted in persistent shoulder pain although the patient had concurrent spondylotic disease with neural foraminal compromise. The left C4 nerve root injury was interesting in that the nerve fascicles were intact suggesting a chance for recovery. There are limited results for reimplantation of completely avulsed nerve roots with peripheral grafts. Dural avulsion without gross nerve root injury is rarely reported.
References:
Haider AS, Watson, IT, Sulhan, S, et al. Traumatic cervical nerve root avulsion with pseudomeningocele formation. Cureus. 2017 Feb 14;9(2):e1028. doi: 10.7759/cureus.1028.
CATEGORY: SPINE // PATIENT WITH CERVICAL SPINE TRAUMA SUFFERS MULTIPLE CONCURRENT PATHOLOGIES
Patient with Cervical Spine Trauma Suffers Multiple Concurrent Pathologies