- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Revision Surgery Relieves Woman’s Chronic Low Back Pain Case Study
Revision Surgery Relieves Woman’s Chronic Low Back Pain
March 11, 2022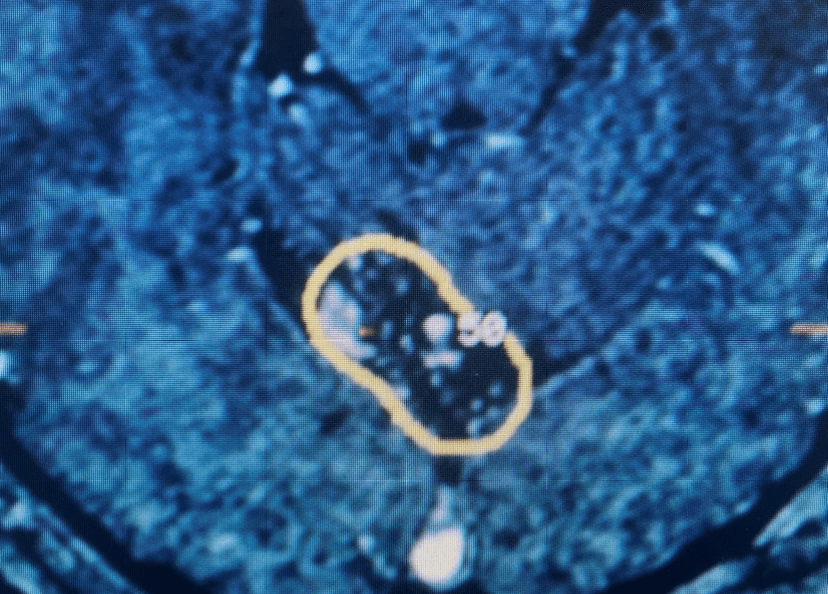
Posterior Fossa Brain AVM – 20-Year Follow-Up
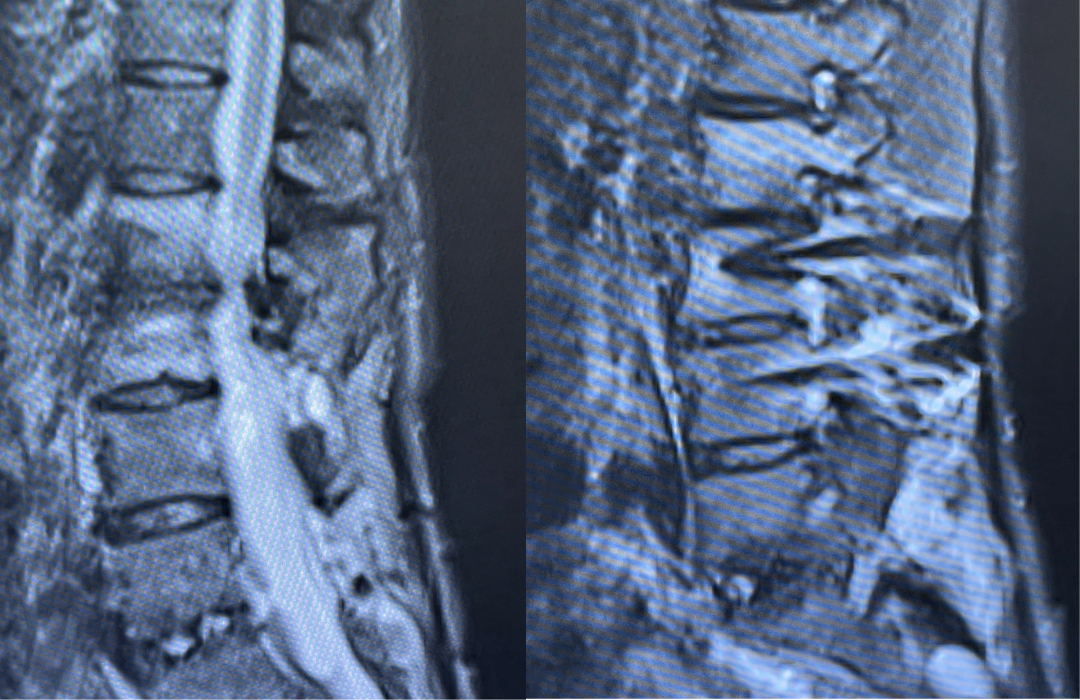
March 21, 2022This 62-year-old female presents with chronic intractable low back pain with radiation down the front of her thighs. The patient had had two prior fusion surgeries: She initially had an L4-S1 fusion twelve years prior and a subsequent revision extension of her fusion at L3-4 that she had three years prior. She had a long-term history of smoking. She had mild hip flexor weakness, right greater than right. Imaging studies revealed next segment degeneration and stenosis at L2-3. (Figs. 1a and 1b and 2).
Figures 1a and 1b. Sagittal T2 MRIs of the lumbar spine demonstrating L2-3 stenosis after L3-4 instrumented fusion.
The patient failed conservative management and was recommended to have a revision decompression with extension of her fusion to L2. The patient underwent a revision L1-L3 decompression with exploration of the lumbar fusion, and removal of the previously placed construct. The fusion was rock solid which was interesting given her extensive smoking history but we had used bone morphogenetic protein to augment her previous fusion.
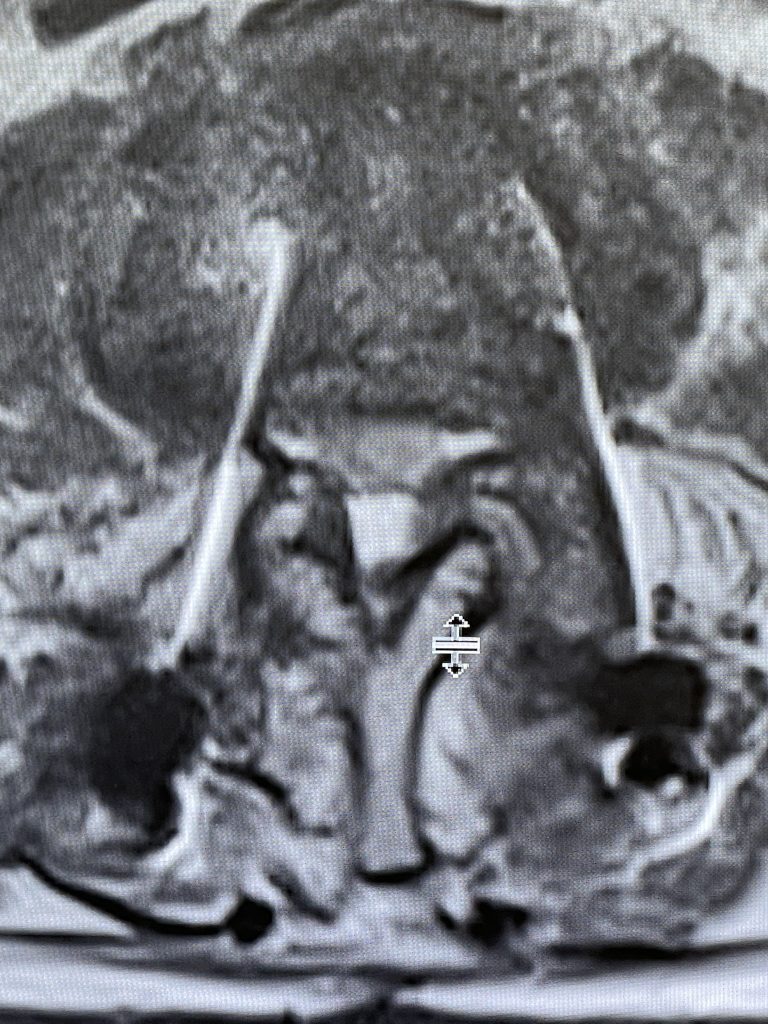
Figure 2. Axial T2 MRI of the lumbar spine demonstrating L2-3 stenosis due to significant facet arthropathy.
During the decompression we removed the inferior facets of L2 after the L3 screws were removed. This is a key maneuver in a revision decompression as it allows access to a dissection plane that allows the foramina and both L3 nerve roots to safely be decompressed. The L2 lamina is removed as well as a dissection plane at the inferior aspect of the bone is developed with an up biting curette. Because of her solid fusion it was only necessary to add new screws at L2 and L3 giving her a shorter construct and less potential stress at the next segment. Post operatively the patient did very well with resolution of leg pain and improved strength in her proximal leg strength. (Figure 3)

Figure 3. Post Op AP and lateral x-rays after L2-3 instrumented fusion
Key Learning points:
Patients who have lumbar fusion surgery are at risk for developing adjacent segment degeneration (ASD) after their index surgery. Patients who develop ASD can have radiographic findings of next segment disease above or below the fusion level. This may consist radiographically of premature disc degeneration, stenosis, spondylolisthesis or retrolistesis, or facet arthropathy. Patients may or may not be symptomatic. The incidence of incidental radiographic findings from many studies ranges from 8-100%. Another analysis of various studies found the rate of asymptomatic ASD to range from 5.2-49%. Patients who have symptomatic ASD is defined as a patient who had relief of their symptoms from the index surgery for a period of time and then develop new symptoms with concurrent correlative radiographic findings. In general, the incidence of development of symptomatic lumbar adjacent level disease ranges from 2-14% per year. Ghiselli et al found the rate of symptomatic degeneration requiring revision surgery to be 16.5% at 5 years, and 36.1% at 10 years after the initial fusion surgery. Risk factors for development of adjacent level disease include but not limited to smoking, BMI, length of fusion construct, disruption of facet complex above during the index fusion, prior degree of disc or facet degeneration and listhesis. Patients who develop ASD with symptoms should be treated with all means of conservative management unless they have a progressive neurological deficit. Revision surgery has attendant risks of a higher incidence of CSF leak as there is scar formation and the anatomy is often distorted. It is important to establish dissection planes early in the surgery with tools such as upbiting curettes. There is controversy whether minimally invasive approaches or dynamic stabilization improves the incidence of adjacent level disease. There are some studies that demonstrate a higher incidence of complications such as durotomy as there are limitations of visualization during minimally invasive procedures. There are some studies that also demonstrate that instrumented fusions have a higher rate of ASD versus noninstrumented fusions. This certainly may be an important consideration in older patients with osteoporosis and comorbidities. Patients who have a long smoking history undergoing fusion surgery would benefit from the use of bone morphogenetic protein.
References:
Lee SL, Hwang, CJ, Lee, SW, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009 Nov; 18(11);1967-1963, doi: 10.1007/s0056-009-1060-3.
CATEGORY: SPINE // REVISION SURGERY RELIEVES WOMAN’S CHRONIC LOW BACK PAIN
Revision Surgery Relieves Woman’s Chronic Low Back Pain