- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Ruptured Dural AV Fistula/AVM of the Posterior Fossa
Middle Meningeal Artery Embolization of Bilateral Subacute Subdural Hematomas
July 22, 2022A Good Solution For Patients With Osteoporosis Who Need Surgery for a “Slipped Disc” or Spondylolisthesis
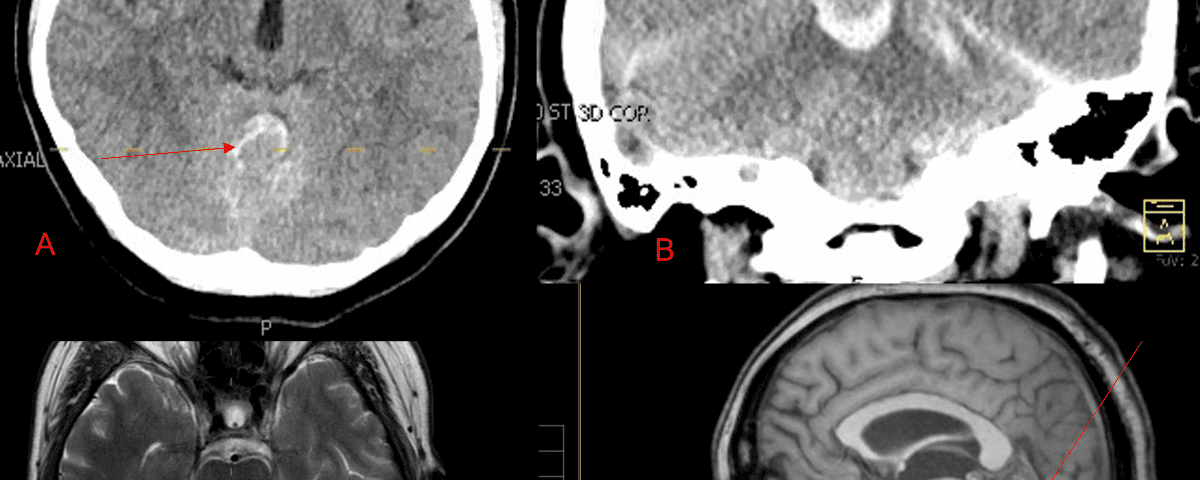
July 24, 2023A 55-year-old woman presented with acute onset of severe headache, and possible witnessed seizure. Imaging confirmed intraventricular hemorrhage primarily focused within the fourth ventricle with diffuse subarachnoid hemorrhage within the posterior fossa and along the tentorium as observed on non-contrast CT and MRI of the Brain (Figure 1).
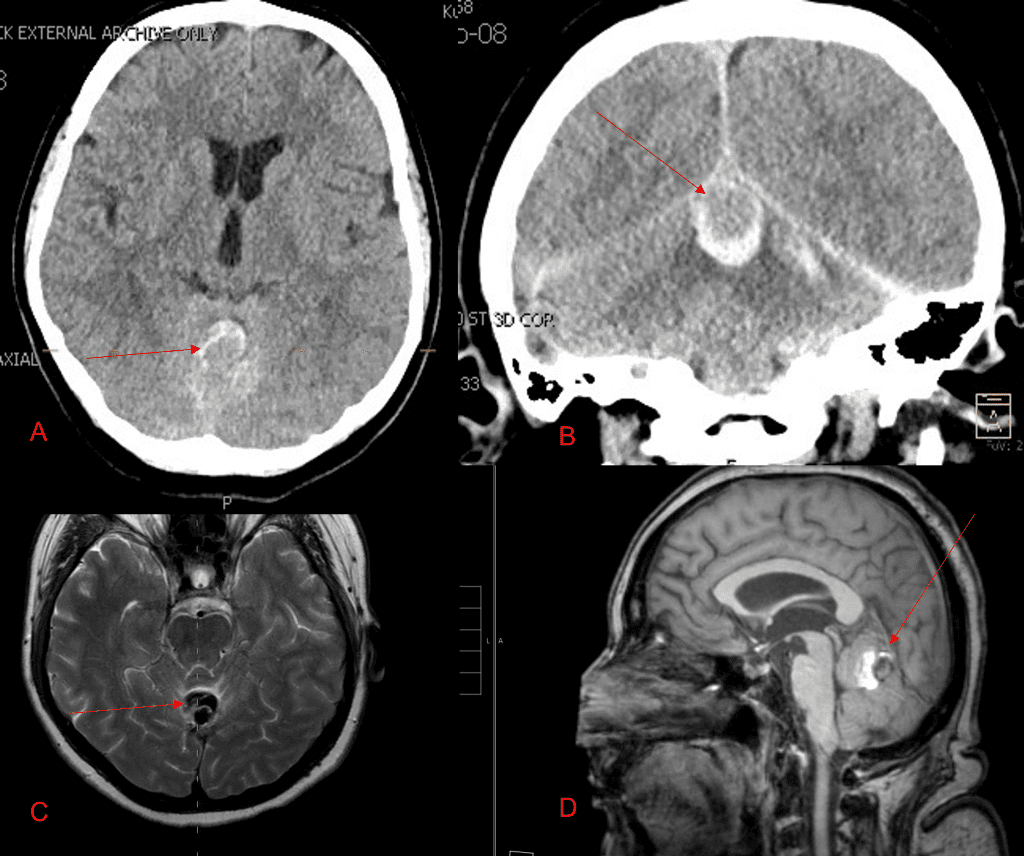
Figure 1. A and B) Non-Contrast CT Axial and Coronal demonstrate large, ruptured Varix/Aneurysm along the Incisura of the posterior fossa which appears to have mixed hemorrhagic components and enhancement on MRI T2 and post contrast imaging (C and D).
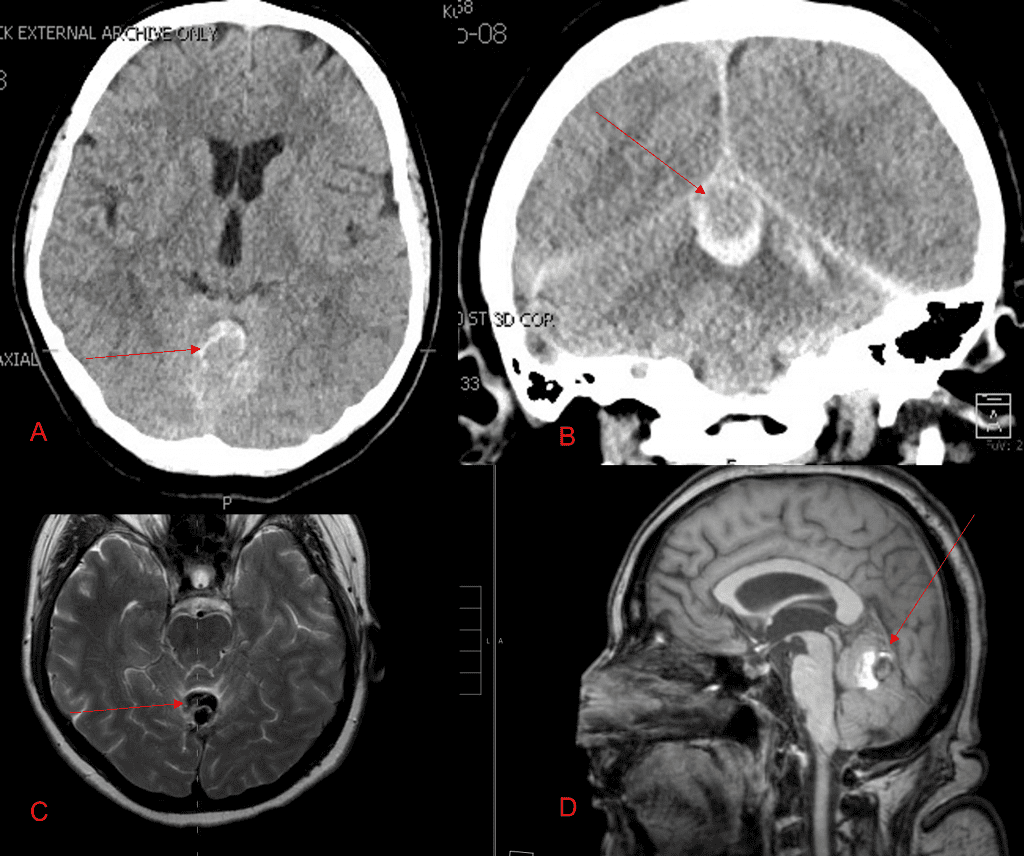
No severe neurologic deficits were observed initially. Her cerebral angiogram revealed a high flow Dural arterial venous fistulous malformation of the tentorium supplied by the bilateral external carotid and left vertebral arteries into a large venous varix within the fourth ventricle at the site of the hemorrhage. Deep venous drainage is observed into the Galenic and Straight Sinus of the posterior fossa (Figure 2).
![[A] Ruptured Varix/Aneurysm of the Deep Venous Posterior Fossa drainage and AV shunting (arrows) [B] Posterior Meningeal Artery Fistula [C] Right Middle Meningeal Artery Fistula [D] Post embolization Left Vertebral Angiogram demonstrates resolution of the high flow and pressure A-V Shunting following successful embolization with liquid embolic (NBCA)](https://nsp-management-services-of-long-island-v1752162808.websitepro-cdn.com/wp-content/uploads/2022/08/figure-2-dural-avmavf.png?nc=4203104367)
Figure 2. [A] Ruptured Varix/Aneurysm of the Deep Venous Posterior Fossa drainage and AV shunting (arrows) [B] Posterior Meningeal Artery Fistula [C] Right Middle Meningeal Artery Fistula [D] Post embolization Left Vertebral Angiogram demonstrates resolution of the high flow and pressure A-V Shunting following successful embolization with liquid embolic (NBCA).

Figure 3. Right ECA AP and Lateral angiograms Pre (A and B) and Post NBCA embolization (C and D) Demonstrate near complete obliteration of right Occipital and Middle Meningeal Artery Fistulas
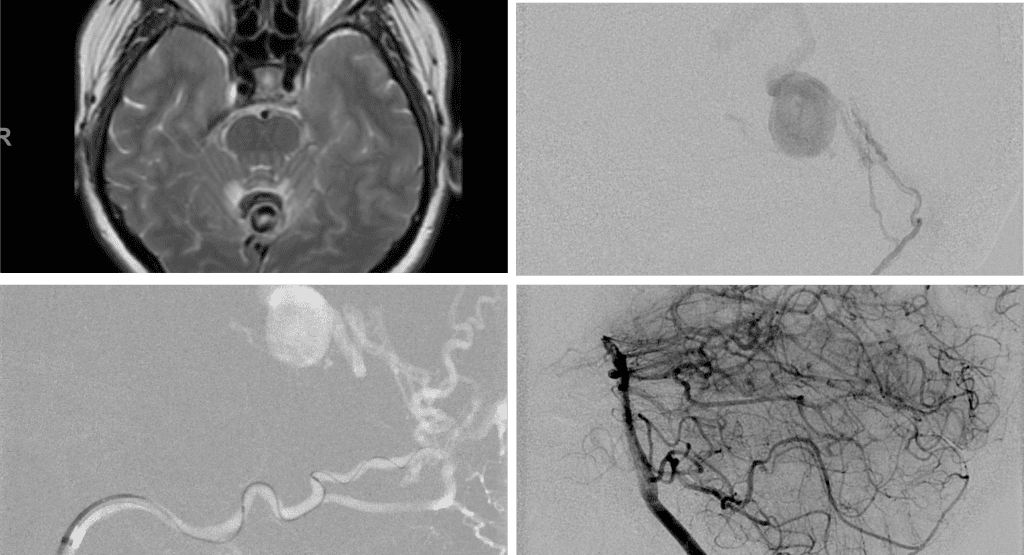
Figure 4. Left ECA AP and Lateral angiograms Pre (A and B) and Post NBCA embolization (C and D) Demonstrate near complete obliteration of Left Occipital Artery Fistulas.
Embolization was successful at immediately reducing the pressure into the Aneurysmal Varix with greater than 90% reduction in A-V shunts. After an intensive period of critical care monitoring and care for her initial brain hemorrhage, she made a near complete recovery with mild intermittent left sided paresthesias and generalized deconditioning. After receiving inpatient and outpatient Acute Rehabilitation, Physical, and Occupational therapy, she completely recovered all of her Activities of Daily Living (ADLs) at 3 months and achieved an modified Rankin Scale (mRS) of 0. On follow-up angiography, small residual low flow A-V shunts were identified and targeted for Gamma Knife Radiosurgery (Figure 5 and 6).
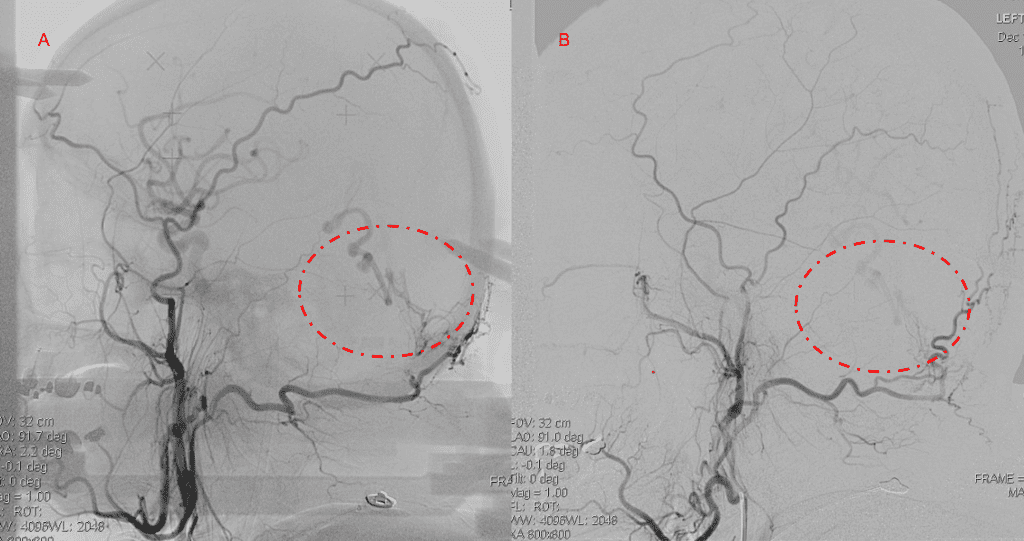
Figure 5. Bilateral ECA Lateral angiograms (A and B) demonstrates small residual indirect supply To the AVM from the bilateral Occipital arteries.
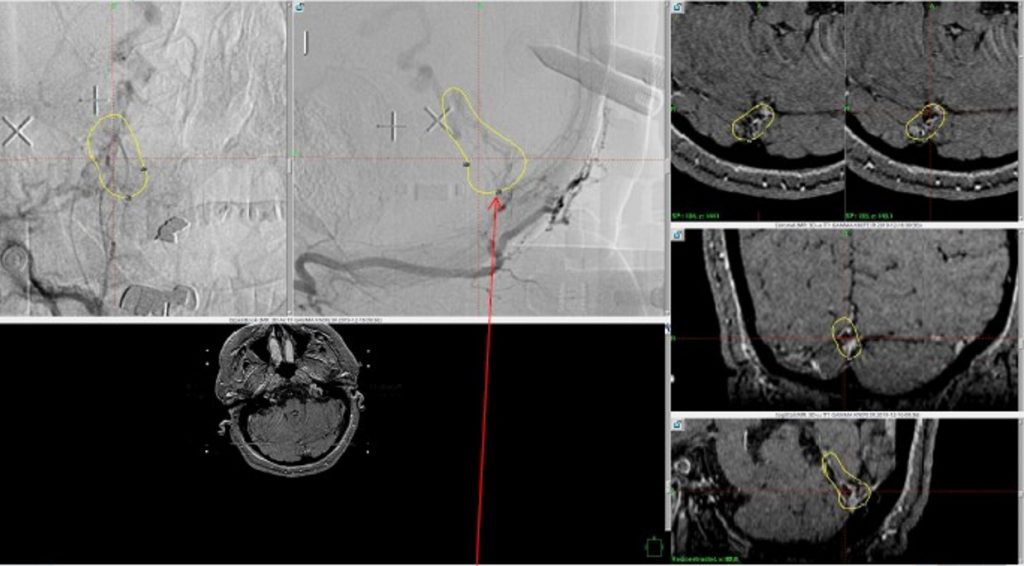
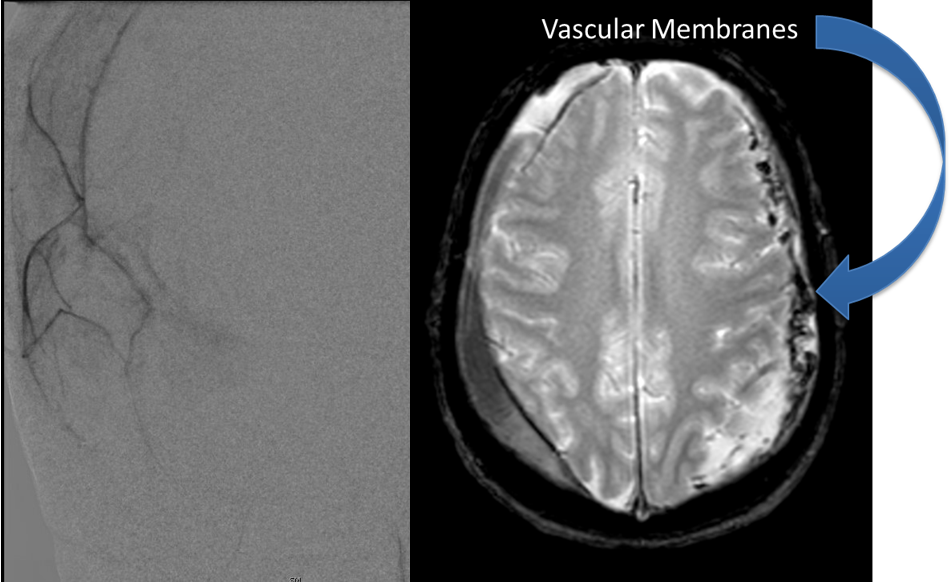
Figure 6. MRI and Catheter Angiograms precisely localize the residual A-V shunts vessels to perform Gamma-Knife Radiosurgery to deliver therapeutic doses to the targets.
Over the 12 to 18 months, she continued to remain event-free and maintain her active independent lifestyle. Delayed angiography over that period confirmed complete obliteration of the Left ECA and Vertebral Artery shunts with near complete obliteration of the Right ECA shunts (Figure 7).
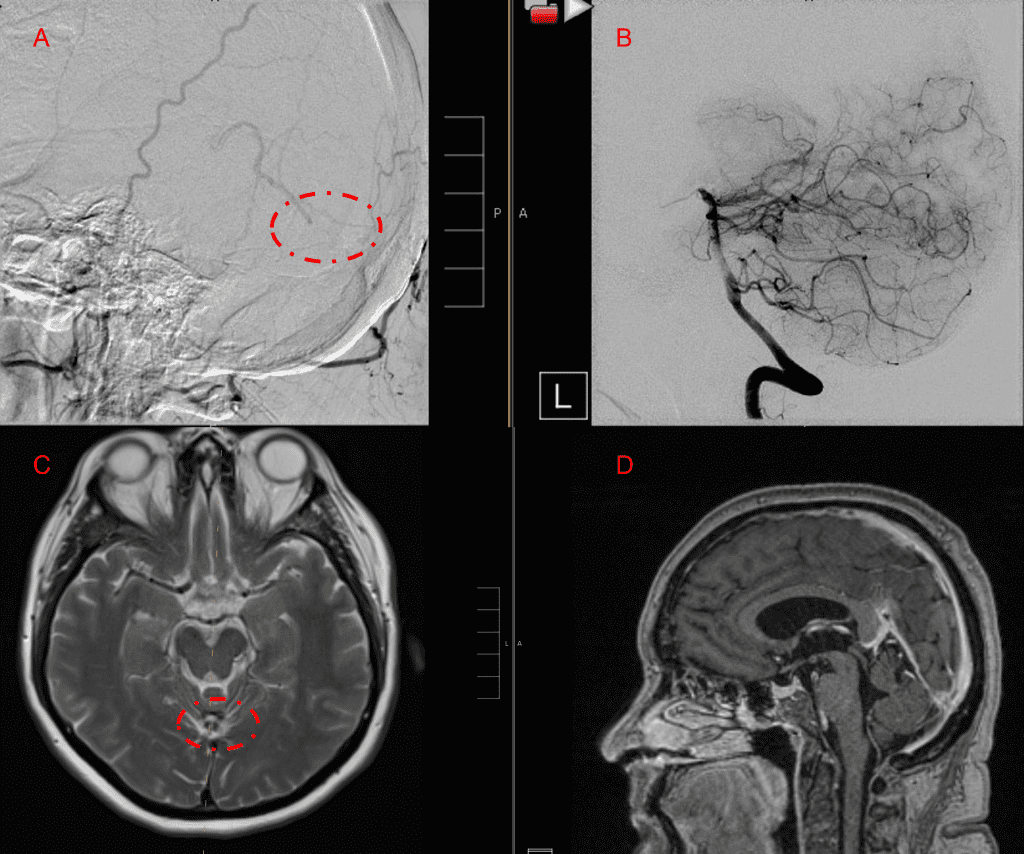
Figure 7. 12 mos follow-up angiograms confirm complete obliteration of the left ECA and Vertebral Supply to the AVM, with a small late-filling component from the right Occipital artery that is markedly Reduced in size and flow (top row). Near complete resolution of the aneurysm and hematoma Is observed on 16 mos post Gamma Knife MRI (bottom row).
Discussion:
Pathophysiology:
Dural Arteriovenous Malformations (DAVM) or Arteriovenous Fistulas (DAVF) are pathological direct vascular shunts from the Dural Arteries to a Dural Venous Sinus or Cortical Vein. Most commonly, they occur independent of Intraparenchymal Pial Brain AVMS, but can sometimes be associated. Most commonly, Dural AVFs are found to be idiopathic, although occasionally can by found to be associated with craniotomy/surgery, trauma, or Dural Sinus Thrombosis. As opposed to Pial Brains AVMs, most DAVFs are often observed in older patients, and generally felt to be acquired or develop over time, the mean age of presentation in the 5th or 6th decade, equal prevalence by gender, although hemorrhage has been reported at a higher incidence in men. A genetic linkage or family history prevalence has not yet been identified.
Classification Systems:
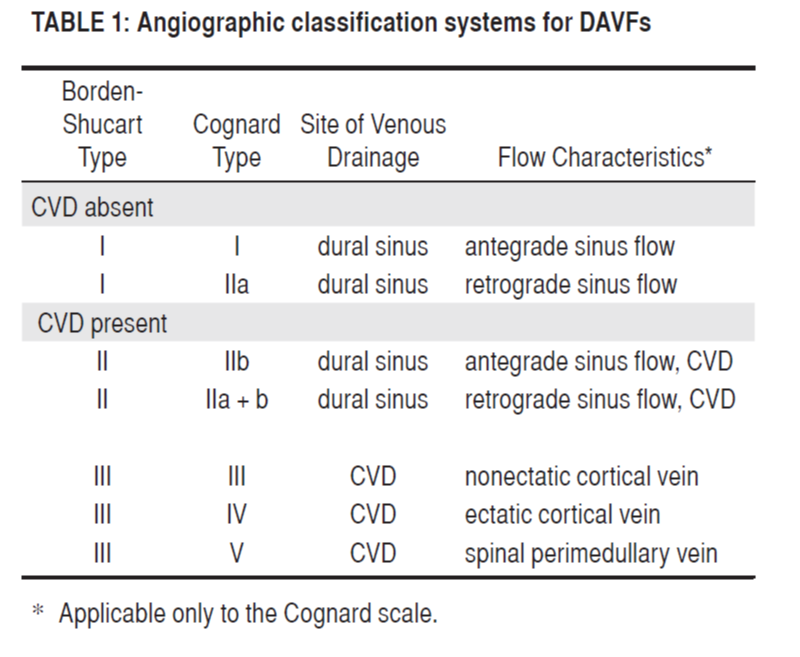
Traditionally, there have been 2 widely used anatomic/angiographic classification systems used to describe Dural AVFs, primarily based on the pattern of venous drainage. The Cognard system was adapted from the original Djinjian system and classifies them based on the direction of venous drainage (antegrade or retrograde), the presence of Cortical Venous Drainage (CVD), and the architecture of the venous outflow. Similarly, the Borden-Shucart system classifies Dural AVFs on the site of venous drainage (Dural Sinus or Cortical Vein), the presence of CVD, and the number of fistula sites[1]. (Table 1)
These original classification systems suggested that as Venous Drainage and CVD pattern progressed through these scales, the natural history risk of brain hemorrhage (ICH) or non-hemorrhagic neurologic deficits (NHND) increased.
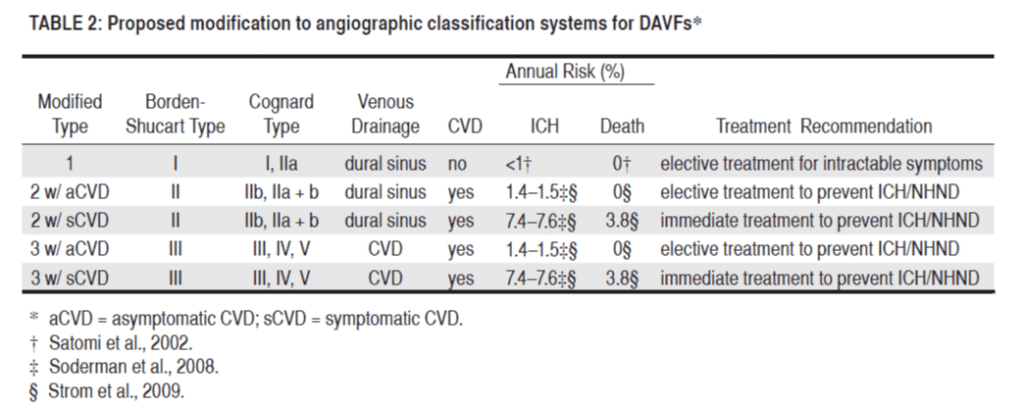
Over the last decade, the neurovascular community has continued to research these patients, and made observations to suggest that the not only the presence of CVD, but the presenting symptoms of ICH or NHND may significantly affect the natural history of Dural AVFs. Zipfel etal. Proposed a new modified classification system which incorporated the presenting symptoms, which suggested a higher rate of ICH (7-8% annually) in patients presenting with CVD and ICH or NHND (termed Symptomatic CVD), than patients with Asymptomatic CVD patients who’s rate of hemorrhage in several retrospective studies was observed to be 1-2% annually (Table 2).1
Management Strategies and Treatment:
Patients presenting with Dural AVMs have a wide range of clinical presentations and may be managed with a variety of treatment strategies. Patients that present without symptoms, or manageable symptoms (ie. Low grade pulsatile tinnitus) and absence of CVD or high-grade features for hemorrhage may be managed conservatively and observed closely over time, clinically and with imaging (MRI, CT, or Angiography). If these patients develop new symptoms or demonstrate evidence of progression and develop high-risk features of CVD or aneurysm formation, then more aggressive treatment can be considered. Many different therapeutic strategies have been successfully utilized to treat safely and effectively high-risk or symptomatic DAVMs. Transarterial embolization of the arterial-venous fistulas using liquid embolic agents (NBCA, Onyx) or particulate agents (Polyvinyl Alcohol) can be used to successfully decrease the number and severity of the high-pressure A-V shunts, effectively reducing the risk of recurrent hemorrhage. In addition, in select cases, and Transvenous approach may be employed to access the anomalous venous structure to embolize the venous recipient of the fistulas and effect a cure. Transvenous embolization must be performed cautiously and in appropriate anatomic and clinical settings to ensure adequate collateral venous drainage. Tentorial DAVMs represent a unique subset of intracranial Dural AVMs. These AVMs are A-V fistulas located in the tentorial dura mater, are supplied primarily by branches of the meningohypophyseal trunk (Tentorial artery of Bernasconi and Cassinari), middle meningeal artery, the occipital artery, and the posterior meningeal artery which often drain directly into smaller pial veins than the less aggressive DAVMs which drain directly into larger venous sinuses (ie Transverse or Cavernous Sinus). Often these AVMS present as higher risk AVMs that are associated with venous aneurysms, subarachnoid hemorrhage, and parenchymal hemorrhage. These tentorial AVMs with their multitude of feeding vessels, CVD, deep location, are extremely difficult to obliterate and may often require a multi-modal staged treatment strategy of embolization, microsurgery, and radiosurgery to effectively reduce or eliminate the pathologic risks of hemorrhagic events.[2]
Stereotactic Radiosurgery (SRS):
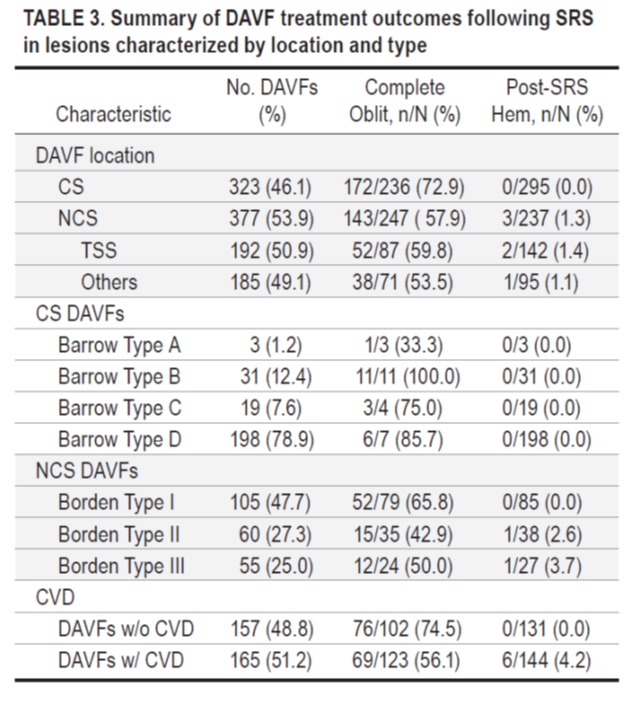
Endovascular therapy and microsurgical therapy offer the opportunity to immediately treat the Dural AVMs and reduce risks. Nevertheless, many DAVMs can not be completely obliterated with either approach secondary to their complexity and deep locations. In these patients, Stereotactic Radiosurgery (SRS) has been successfully applied to residual and high-risk surgical lesions to effectively obliterate them over time (1-3 years is often required for the radiation effects to be achieved). The SRS modalities most commonly used are Gamma Knife Surgery (GKS) and Linear Accelerator (LINAC) – based radiosurgery. Chen et.al. performed a comprehensive review of nineteen studies that studied the complete obliteration rates and hemorrhage rates following SRS for these DAVMs based on their location, grade, and presence of CVD. As Table 3 illustrates, SRS has been successfully in obliterating greater than 50% of these more complex DAVMs, as well as significantly reducing the risk of hemorrhagic events in the observed follow-up period for these patients.[3]
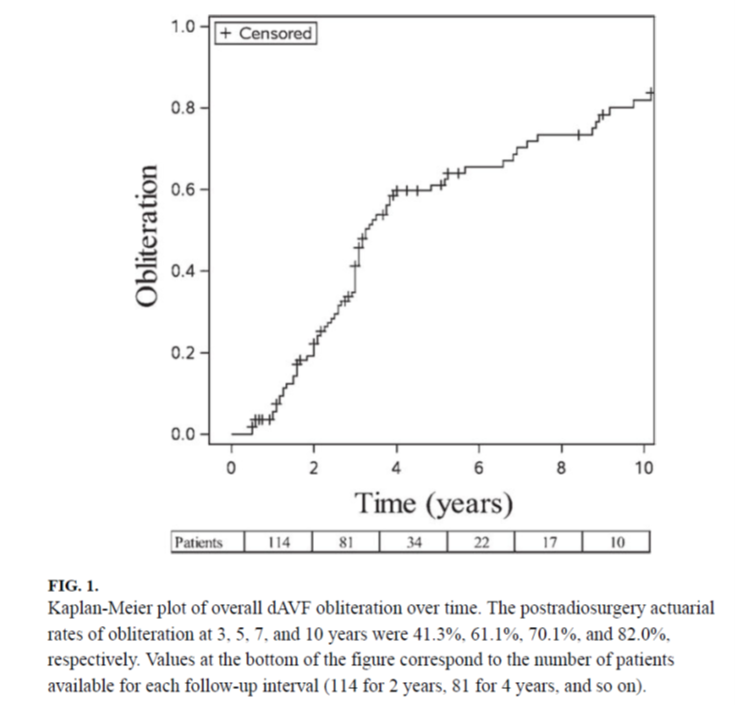
A recent study analyzed the role of Gamma Knife SRS in a data cohort of 114 patients who underwent GKRS for cerebral Dural AVMs from the International Gamma Knife Research Foundation. A mean margin dose of 21.8 Gy was delivered. The mean follow-up duration was 4 years (range 0.5–18 years). The overall obliteration rate was 68.4%. The post radiosurgery actuarial rates of obliteration at 3, 5, 7, and 10 years were 41.3%, 61.1%, 70.1%, and 82.0%, respectively (Figure 1). Post-GRKS hemorrhage occurred in 4 patients (annual risk of 0.9%). Radiation-induced imaging changes occurred in 10.4% of patients; 5.2% were symptomatic, and 3.5% had permanent deficits. Favorable outcome was achieved in 63.2% of patients.[4]
Key Learning Points:
1. Indirect Dural AV Fistula Vascular Malformations represent high risk lesions that result from acquired and/or congenital indirect fistula and A-V shunts that can arise within many of the deep venous structures of the brain (Superficial and Deep Venous Drainage systems).
2. Many patients may present with initially mild symptoms of pulsatile tinnitus or headaches but may progress over time to more severe high-risk symptomatology including hemorrhagic stroke, permanent neurologic deficits, and even mortality.
3. Embolization is a well-established safe and effective treatment to reduce or obliterate Dural A-V Fistulas and AVMs to reduce the risk of recurrent hemorrhage and associated morbidity
4. Gamma Knife Radiosurgery has demonstrated successful and durable treatment of many Brain AVM’s when effectively selected and targeted.
5. Early evaluation by an expert multi-disciplinary team is critical to diagnosis, management, and successful treatment and recovery with a variety of medical, endovascular, and surgical approaches.
References
[1] Zipfel GJ, Shah MN, Refai D, Dacey RG Jr, Derdeyn CP. Cranial dural arteriovenous fistulas: modification of angiographic classification scales based on new natural history data. Neurosurg Focus. 2009;26(5):E14. doi:10.3171/2009.2.FOCUS0928
[2] Lewis AI, Tomsick TA, Tew JM Jr. Management of tentorial dural arteriovenous malformations: transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg. 1994;81(6):851-859. doi:10.3171/jns.1994.81.6.0851
[3] Chen CJ, Lee CC, Ding D, et al. Stereotactic radiosurgery for intracranial dural arteriovenous fistulas: a systematic review. J Neurosurg. 2015;122(2):353-362. doi:10.3171/2014.10.JNS14871
[4] Starke RM, McCarthy DJ, Chen CJ, et al. Evaluation of stereotactic radiosurgery for cerebral dural arteriovenous fistulas in a multicenter international consortium. J Neurosurg. 2019;132(1):114-121. doi:10.3171/2018.8.JNS181467