- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Spinal Dural Fistula Causing Myelopathy & Incontinence: Reversal After Endovascular Embolization

Spinal Embolization Treats Aggressive Compressive T3 Vertebral Body Hemangioma
October 27, 2021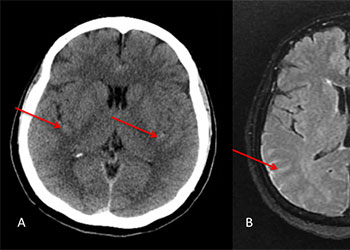
Ruptured Thoracic Spinal Arterial Dissecting Aneurysm
October 27, 2021The patient is a 65-year-old woman with a history of hypertension and hypercholesterolemia who was experiencing bilateral lower extremity weakness and numbness for close to one year in addition to some urinary incontinence for the preceding 6 months. The patient ultimately saw a neurologist who ordered an MRI of her lumbar sacral region revealing a bright signal within the lower spinal cord on T2-weighted sequences with enhancement and flow voids seen on the dorsal aspect of the spinal cord suggestive of spinal dural arteriovenous fistula (Figure 1). She was referred for a neurovascular consultation. Physical examination was significant for 4/5 weakness on the right hip and leg muscle groups with decreased pinprick and light touch sensation in both lower extremities in a stocking distribution and decreased vibratory sensation in both toes.

(Figure 1) Pre-treatment MRI image of lumbar sacral region.
Based on the MRI findings and the clinical presentation, a spinal dural fistula was presumptively diagnosed and a spinal angiogram recommended with planned attempt to embolize a fistula if encountered. Spinal angiography confirmed a spinal dural fistula fed from radiculomedullary branches off the left T6 pedicle and draining into a spinal vein (Figure 2B & 2D).
No spinal arteries were identified from this pedicle and after provocative testing with lidocaine and amytol injection confirmed that no arterial input to the spinal cord, the fistula was sealed with one injection of onyx glue (Figure 2C). Post-embolization angiogram confirmed no residual filling of the fistula (Figure 2D).
Post-operatively the patient did well and at follow-up reported increased strength in her legs and decreased bowel and bladder dysfunction.
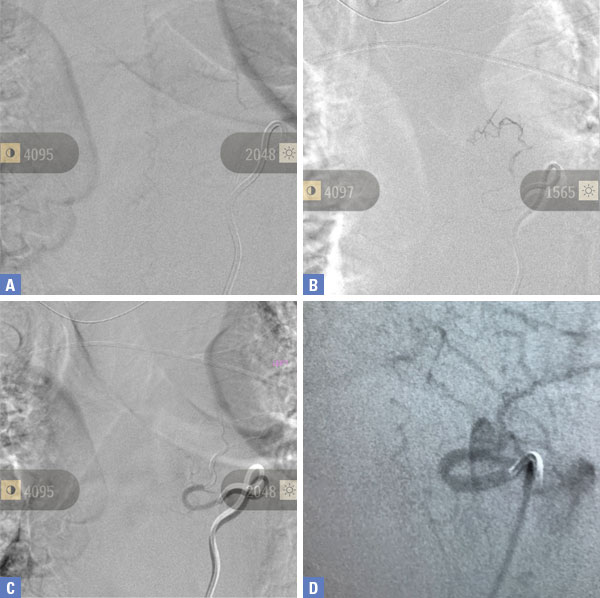
Pre-Treatment (Figure 2A and 2D), At Treatment (Figure 2B – Onyx Glue Cast), and PostTreatment (Figure 2C)
Spinal dural fistulas are rare but important disorders treated by neurovascular neurosurgeons.
They are much less common than brain arteriovenous malformation and even less common than dural fistulas of the brain, themselves rare lesions. Typically presenting in older individuals, these lesions can mimic spinal degenerative stenosis with several distinguishing features. Insidious weakness out of proportion to pain are hallmarks of spinal fistulas and can be used to differentiate this disorder from degenerative disease.
MRI with contrast is the usual diagnostic as the enhancement and bright signal on T2-weighted imaging reveals spinal cord venous congestion from inappropriate arterial input. Both endovascular embolization and microsurgical clipping are relatively safe and effective treatment with the degree of recovery correlated with the duration and severity of symptoms. It is my practice to attempt embolization as the first line of therapy. If this is either not accomplished or the fistula is not closed significantly and clinical symptoms persist as happens on occasion, surgical ligation is performed.
CATEGORY: ENDOVASCULAR // SPINAL DURAL FISTULA CAUSING MYELOPATHY & INCONTINENCE: REVERSAL AFTER ENDOVASCULAR EMBOLIZATION
Spinal Dural Fistula Causing Myelopathy & Incontinence: Reversal After Endovascular Embolization



