- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Spinal Embolization Treats Aggressive Comprehensive T3 Verterbral Body Hemangioma
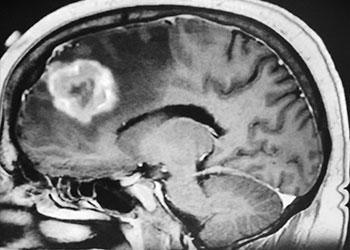
Brain Metastasis
October 26, 2021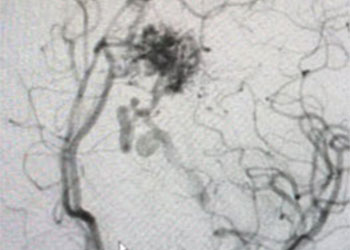
25 year old woman with Brain AVM (arteriovenous malformation)
October 26, 2021
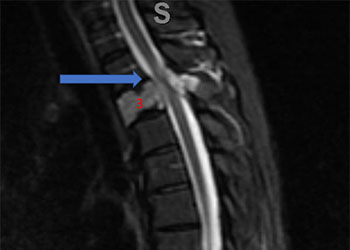
Figure 1. A) Sagittal T2 MRI demonstrates aggressive hyperintense T3 hemangioma involving the body and posterior elements compressing the thoracic spinal cord (arrows)
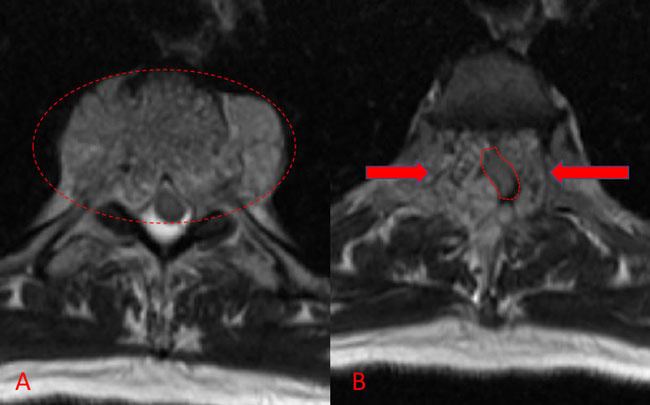
Figure 1. B and C) Axial MRI images of T3 demonstrates extensive infiltrative lesion with extradural compression of the thoracic spinal cord. (Dashed lines in A) tumor infiltration; Dashed lines and Arrows in B) cord compression.
Significant spinal cord compression was identified with no other bony lesions in the entire spinal axis. Metastatic work-up was also negative. A diagnosis of vertebral body hemangioma, an aggressive subtype, was made and spinal surgery consultation obtained. Our neurosurgical team was consulted for preoperative embolization of the tumor prior to surgical decompression and instrumented fusion.
Spinal angiography showed a very hypervascular lesion fed predominantly by the right supreme intercostal artery (Figure 2. A, B).

Figure 2. (A, B) Selective angiography of the right supreme intercostal artery demonstrates extensive hypervascularity of this aggressive T3 hemangioma.
No spinal artery contributions were found to arise from this right T1-T3 pedicle. Superselective WADA testing was performed with Brevital injected through the microcatheter, which failed to elicit changes in the intraoperative monitoring, confirming safety to proceed with devascularization of this pedicle and tumor. This was performed with 100-300 micron particles achieving an excellent devascularization (Figure 3. A, B).
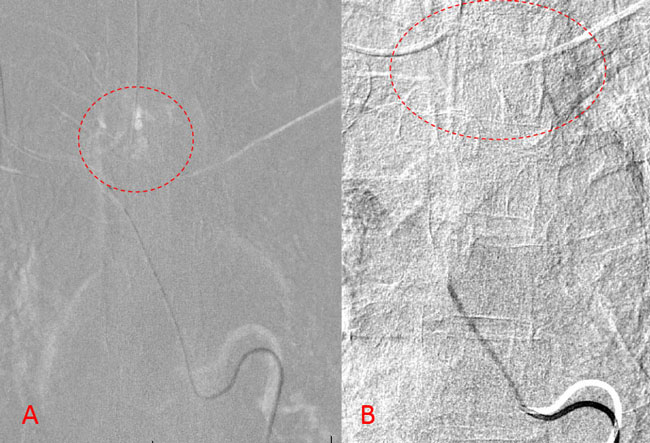
Figure 3. A and B) demonstrates selective PVA embolization with complete devascularization of the tumor on completed embolization.
The patient underwent a safe and successful posterior decompression with corpectomy and instrumented fusion with minimal blood loss and discharged home with reversal of neurologic deficits and resolution of symptoms.
DISCUSSION:
Hypervascular lesions of the spinal axis can be very challenging lesions that can result in significant morbidity when presenting with growth, expansion, and cord compression. Surgical decompression is often urgently needed, but can be complicated by extensive hemorrhage, limiting visualization of the surgical field and increasing the risks of adverse events or cord injury during surgery. Preoperative embolization is often recommended prior to surgical therapy for these lesions, especially in the settings of hypervascular metastasis (i.e. renal cell, myeloma) or primary vascular tumors such as hemangiomas as in this patient. Embolization can be performed safely via a transarterial route in most patients, with superselective angiography of the feeding pedicles and if needed, provocative WADA testing with short acting anesthetics (Amytal, Brevital, Lidocaine) to exclude high risk contributions to the spinal cord vascular supply. Embolization can then safely be performed with particulate, liquid, and coil embolization as desired. In some patients, trans-arterial access may be limited, and direct puncture approaches to the tumor can also be considered in the spinal axis as well aggressive lesions of the head and neck (References 1-3).
REFERENCES:
CATEGORY: ENDOVASCULAR // T3 HEMANGIOMA COMPRESSES THORACIC SPINAL CORD
Spinal Embolization Treats Aggressive Comprehensive T3 Verterbral Body Hemangioma
A 54 year-old man presented with mid-thoracic back pain and was found, by imaging, to have a presumed T3 vertebral body hemangioma. He was neurologically intact and treated conservatively without further medical attention for this lesion.
He presented to the emergency room with one-week history of thoracic pain in addition to bilateral lower extremity weakness and paraparesis. MRI imaging with contrast showed a diffuse abnormal signal within the vertebral body of T3 and the posterior elements with lobulated soft tissue lesion extension into both paraspinal areas (Figure 1. A, B, C).