- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
IMPORTANT CONSIDERATIONS IN SPINE SURGERY

SOMETIMES YOU HAVE TO CONNECT THE SKULL TO THE NECK
May 23, 2024Dr. William Sonstein Launches New Podcast
September 11, 2024
I had some time off to contemplate nature and the beauty of Alaska and took a break from neurosurgery. I think it’s very important to take time to remember the other things you do besides your job. I’m back and we’ve been pretty busy since I got back from vacation. We have done some interesting cases starting with a two-level anterior cervical discectomy on a young female who had an interesting presentation of her problem.
This 30-year-old female presented with neck and parascapular pain. She had initially had an MRI of the cervical spine (Fig. 1) which demonstrated a herniated C5-6 disc with a central component and more eccentric off to the left. She had initially improved with steroids but then developed pain down her right arm which became unrelenting despite conservative treatment. This was strange considering her initial MRI showing the disc off to the left.
When she presented, she had significant weakness of her right biceps, triceps, and finger extensors. Because of this discrepancy between her clinical presentation and the MRI findings, a new MRI was obtained which was approximately 5 months from her initial MRI (Fig 2). Her new MRI showed that she had a new 6-7 extruded disc fragment with severe right foraminal stenosis and a less prominent C 5–6-disc herniation.
Clearly this explained her right upper extremity symptoms. Because of her weakness, it was decided to perform an anterior cervical discectomy at C5-6 and C6-7 and interbody fusion with plate. An extruded disc was found at C6-7. The patient did well postoperatively with improvement of her radiating pain and strength (Fig 3). This case illustrates the importance of repeating an MRI if the symptoms and signs do not correlate with the MRI findings. Disc herniations can change. They can be reabsorbed, and they can also worsen over time.
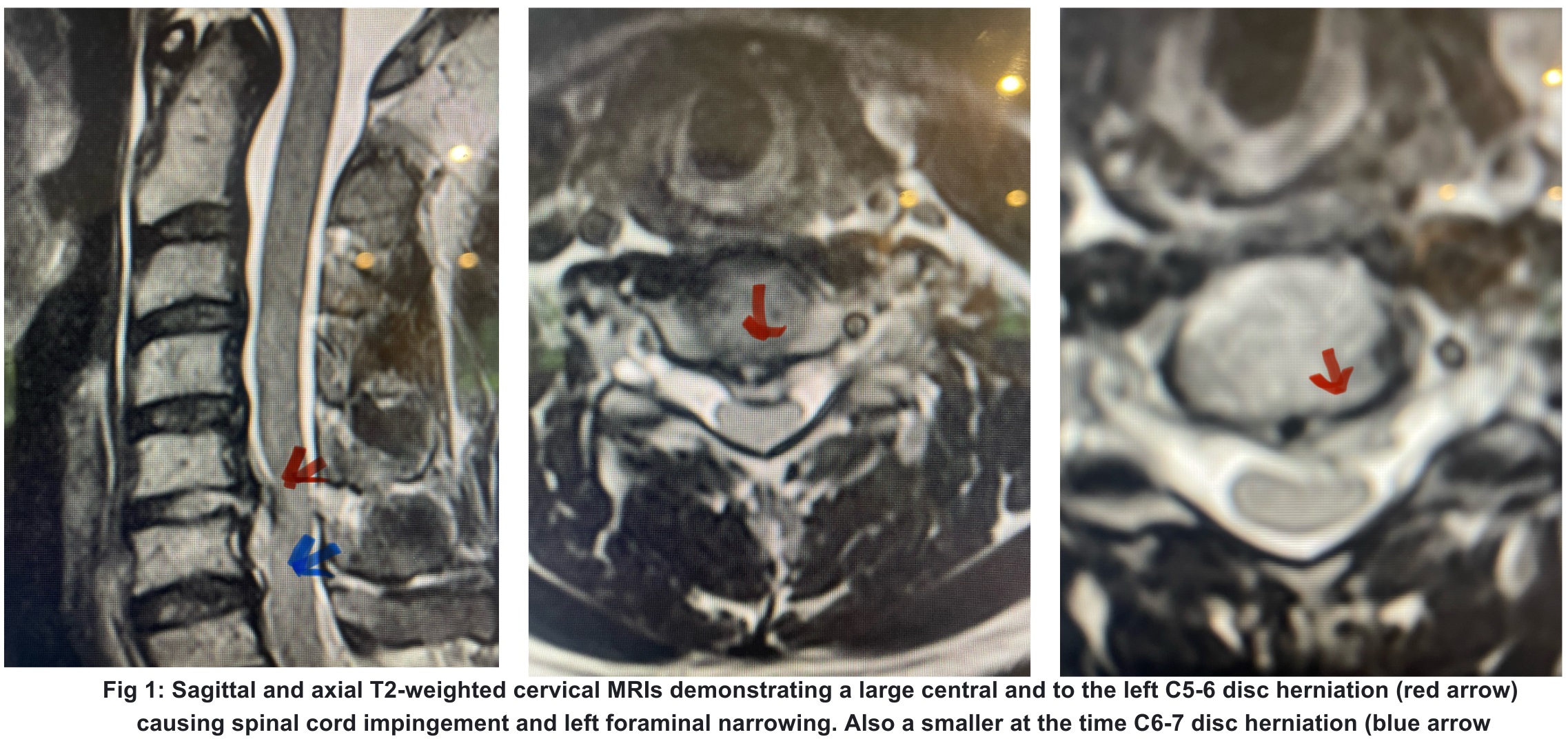
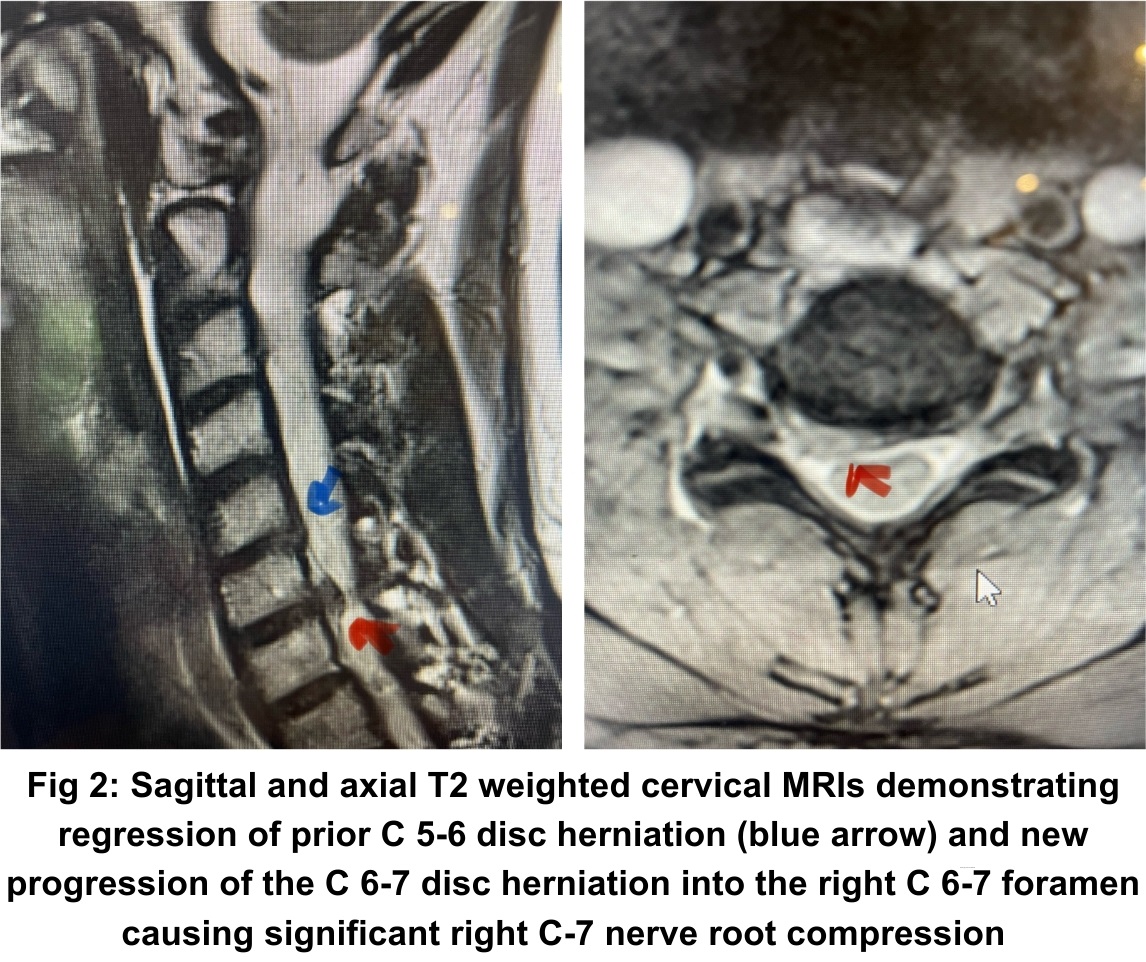

Fig 3: Intraoperative lateral cervical x-ray demonstrating good placement of the C5-C7 interbody cages and plate (red arrow)
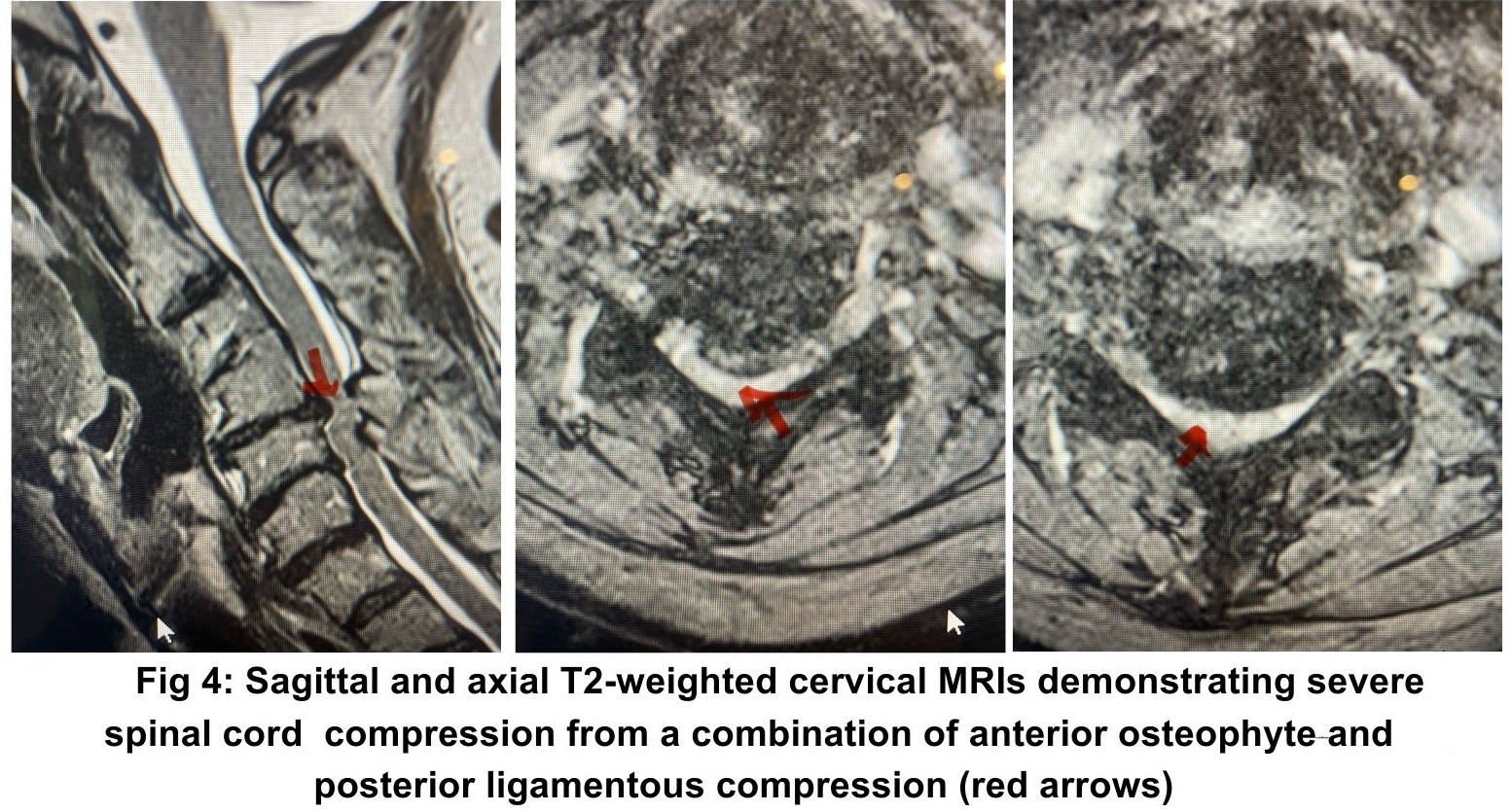
Another case was a 75-year-old female, who for about a year has had difficulties with her hands. She complained of numbness and weakness of her hands with some balance dysfunction. MRI revealed severe cervical stenosis, centered mainly at C4-C6 (Fig 4). There was both anterior and posterior contribution to the stenosis.
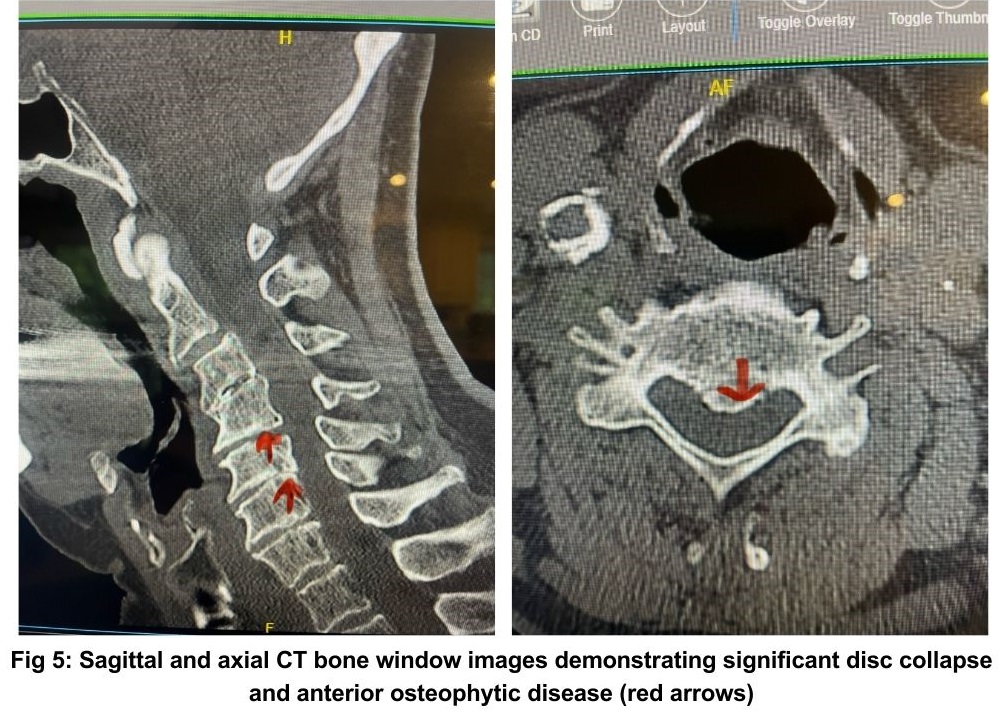
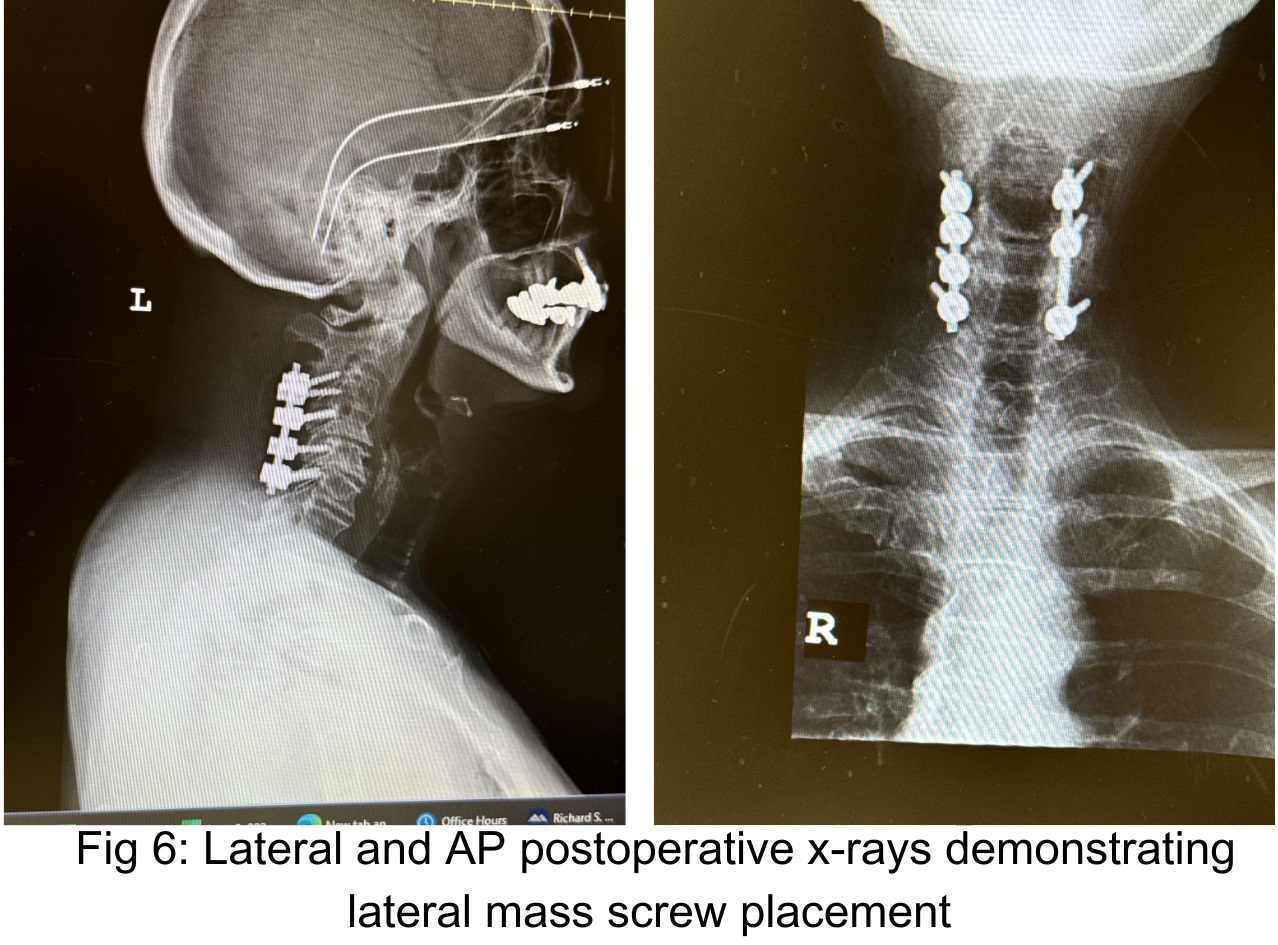
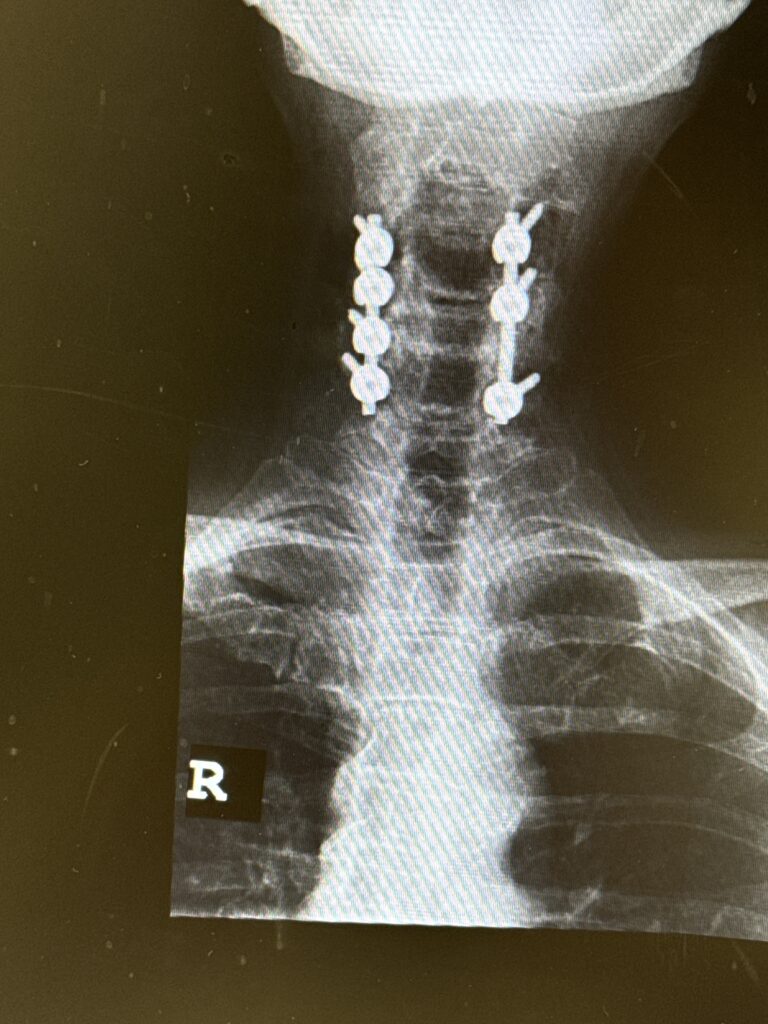
Although her upper cervical spine had a relative kyphosis, her mid and more inferior cervical spine curved into a more neutral to slight lordotic curve. Because she had significant degenerative collapse of her C4-6 segments anteriorly, and calcific compression anteriorly (Fig 5), it was decided to perform a posterior C3-C7 decompression of her spinal cord and a C3-C6 fusion with instrumentation to preserve her alignment (Fig 6).
We felt that the area of most concern could be approached posteriorly because the affected area of the cervical spine had a relative lordosis. A posterior approach to a kyphotic segment is not favorable because one can biomechanically worsen anterior neurological compression. It would be more difficult anteriorly because of her collapse of the disc space in order to get an adequate full decompression since she had significant posterior disease and compression. Because she had a relative lordosis a full decompression could be accomplished in our opinion better by a posterior approach.