- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
My Love For Picking Arthritis Off The Dura
Neuropathic Face Pain Syndromes – Non-Invasive Treatment Options
December 2, 2022Great News for NSPC Patients – You’re Protected from Out of Network Bills
April 4, 2023
th
After 25 years in practice, I still find it challenging, but quite rewarding: removing degenerative material off the dural membrane in the lumbar spine. Some people have membranes that are so floppy and thin, particularly older women. However, we love the art of essentially picking this material off the dura and especially when we have a thick membrane! Having a fantastic, experienced partner that assists expertly in retracting away this parchment-like membrane to clear a safe plane is the key to a great result which I fortunately have. The art of “touch” is most critical; knowing the right downward pressure. Knowing what you can bite, knowing what you can lift and what you can stretch. What really is the ideal tension you can safely get away with. Sometimes shoveling is a great move. Using the Kerrison, smooth on one side and sharp biting on the other, you find the right plane, clearing the dura and shovel the thick ligament upward off the dura and during the same maneuver, detach it from the bone then you can safely remove it with a bite. We do everything we can to do this safely and try to avoid violating the membrane like the plague. If this occurs we fix it with a stitch and some biological glue. This is the art, this is the challenge, and we take it very seriously. This is our job and we love doing it but I do not think people really fully comprehend what we go through to get the job done, both emotionally and physically, in order to decompress these patients who have a very narrow spinal canal due to this arthritis build up. In technical terms this narrowing of the round canal is called lumbar stenosis. Again arthritis is just a compensatory mechanism for chronic instability. The word chronic is key because it takes years to develop this. When the disc degenerates and when the ligaments become lax, the spine is signaled to make stabilizing structures: enlarged joints, calcified extensions, thickened ligaments which are just forms of arthritis. In the process of the spine trying to take care of its own stability, the nerve sac and nerves become collateral damage.
Patients with lumbar stenosis most commonly have pain, numbness, and heaviness of their legs that gets worse when they walk or stand and improves with sitting or flexing forward. Most importantly does their MRI correlate with their symptoms and/or exam? If they have L4-5 stenosis, do they have weakness of their dorsiflexion? At the level of stenosis, is the stenosis eccentric and if so, does that side correlate with the side of their symptoms? However, even on axial MRI images if one side is more affected, although both sides are to some degree, the symptomatic side does not need to be on the worst side of stenosis. This is because a bony compression on one side can compress the opposite side against the bony ring.
If a patient with lumbar stenosis with symptoms that correlate with the MRI findings, and they have failed all conservative treatments, and their lifestyle is being affected, what can we do? We can offer a patient a procedure called a lumbar laminectomy. Patients are always asking me what this actually is. In medicine “ectomy” means to remove so therefore we “remove” the lamina. The back portion of the spine which is like the roof of the spine consists of a bony process that sticks backward called the spinous process and two symmetrical flat pieces of bone that cover the remainder of the thecal sac. Then on either side of the lamina there are two joints called the facet joints which cover the exit zone of the nerves. These are like any other joints like hip or knee joints and can become enlarged and are the main culprits that close in the walls of the canal, generally resulting in a triangular or trefoil shape. For a patient with severe concentric stenosis, a laminectomy is conducted which removes the spinous process, lamina, and a portion of the facet joint to fully decompress the sac of nerves and the descending nerve into the nerve canal or foramen. I use two main instruments which are biting instruments, the Leksell rongeur, for more gross work, and Kerrison punch, for more finer work (Fig 1)

(Figs 1a) Demonstrating Kerrison punch for decompressing the spinal canal

(Figs 1B) Leksell rongeur
These are used to remove the roof of bone over the spinal canal by essentially “biting” away the bone. The art and experience with this comes with learning a certain touch and controlled removal of the bone without undo downward pressure. It is important to know “when” to release the tissue, without any pull on the thin attachments to the dura that could cause a tear. It is imperative that as you are removing the bone and thickened ligament in order to make the canal round again, your assistant is gently retracting the dura with a smooth dissector in order to dissect a plane that is clear for the Kerrison punch.
The goal is simple: make the thecal sac round again and to open the nerve tunnel or foramen to make the nerve root loose. This is achieved by removing bone to enlarge the dimensions which is the laminectomy and foraminotomy and shaving away the arthritis using our special tools. Here are some illustrative cases that are in need of decompression using these techniques.
This 57 year-old male had a long history of low back pain and left lower extremity pain and numbness. The patient had failed conservative treatment of physical therapy and epidurals. MRI revealed tight left L2-3 and L3-4 lateral recess stenosis as well as significant right L4-5 facet arthropathy and right lateral recess stenosis as well as a grade 1 L4-5 spondylolisthesis

(Fig 2) Sagittal T2-weighted lumbar MRI demonstrating (arrow) tight lateral recess stenosis

It was felt that the patient should undergo surgical decompression and fusion at L4-5 given his spondylolisthesis. Post operatively he had an uneventful course and he had relief of his leg pain.
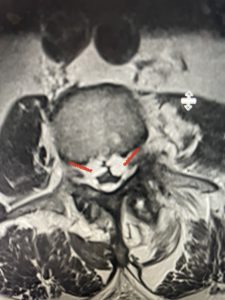
The next patient is a 71 year-old male with a two-year history of low back pain and lower extremity pain, numbness and weakness. His left leg was worse than the right. He had had five epidurals with no improvement. He also had tried physical therapy and medicines but nothing helped. He also felt that over the last three weeks he had gotten worse. He also had recently had some decreased sensation of bladder fullness and difficulty with bowel movements. MRI revealed a very tight L2-5 stenosis with an extruded L3-4 disc fragment (Fig 3).

(Figs 3a) Sagittal (a) and Axial (b) T2-weighted lumbar MRI demonstrating severe spinal stenosis L2-5 (arrow)and extruded disc at L3-4 on axial image (arrow)
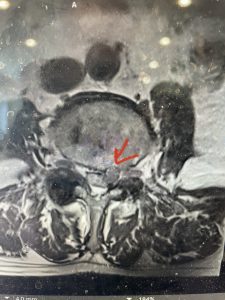
(Fig 3b)
He had concentric severe stenosis with severe compression of the lateral recess and foramen at L3-4 secondary to the superimposed disc herniation. The fact that he had gotten worse with subtle cauda equina features with an extremely tight canal, he underwent a decompressive laminectomy. We also augmented his laminectomy with an in situ fusion from L3-5 as he was relatively young, with more time to reform arthritis, and had been unstable enough to extrude a disc fragment. By placing “bone dust” or bone material along the sides of the spine, specifically laying it across the transverse processes after they have been drilled to bleeding bone, you provide an environment where bone formation is induced to connect the segments, stabilize them, and thereby reduce the signal to make more arthritis as that signal is still present despite the laminectomy. What was interesting was that we encountered a large extruded disk fragment that was significantly contributing to his compression which is often not found in patients in this age bracket. Post operatively he had much improvement of leg pain.
This 66 year-old male with Factor XI deficiency had originally had a decompressive laminectomy L2-S1 and in situ fusion about three years prior for severe thecal sac compression mainly due to severe epidural lipomatosis (Fig 4).

(Fig 4a) Sagittal (a) and Axial (b) T2-weighted lumbar MRI demonstrating severe spinal stenosis L2-5 (arrow)and extruded disc at L3-4 on axial image (arrow)
(Fig 4b)
Epidural lipomatosis is a relatively rare condition where normally present fat in the epidural space is hypertrophied and can cause severe thecal sac compression. It is generally deposited more in the lateral and dorsal epidural space. This can be caused by long term steroid use and obesity, but also can be idiopathic. He had done well until more recently had developed low back pain with bilateral thigh pain and numbness. He had difficulty walking because of the pain. A new MRI (Fig 5) revealed that he had developed severe degeneration of the L1-2 segment above his prior decompression and fusion with a large extruded disc/osteophyte, right greater than left with severe thecal sac compression. He also had some residual T12-L3 residual epidural lipomatosis.
He had failed conservative treatment consisting of neurontin, physical therapy and epidural injections. He underwent revision laminectomy T12-L3 to decompress and explore prior fusion. He did have significant epidural fat encountered particularly at L1-2. The fat in epidural lipomatosis has a much more firm, globular texture. It takes a while to search within the fat, gently dissecting with a Penfield 4, to finally find the thecal sac! We encountered a large subligamentous extruded fragment lateral to the thecal sac on the right above the take off of the L2 nerve root. We removed any more residual fat at the L2-3 level and T12-L1 and decompressed the sac well. On exploration of the prior fusion it was fairly solid, but had some gaps at L2-3 fusion mass. Therefore we added a T12-L3 in situ fusion to augment those gaps and because we were at the thoracolumbar junction we extended fusion to T12. Post operatively he had relief of his leg pain.

(Figs 5a): Sagittal (a) and axial (b) T2-weighted lumbar MRI demonstrating status post lumbar decompression and insitu fusion L2-5 now well decompressed (blue dash) with development of new (red arrow) severe stenosis and with superimposed right L1-2 disc herniation (blue arrow)
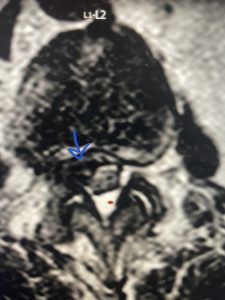
(Figs 5b)



