- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Revision Lumbar Surgery
Lateral Disc Herniations
August 23, 2022Neuropathic Face Pain Syndromes – Non-Invasive Treatment Options
December 2, 2022
fig3 IMG 7141

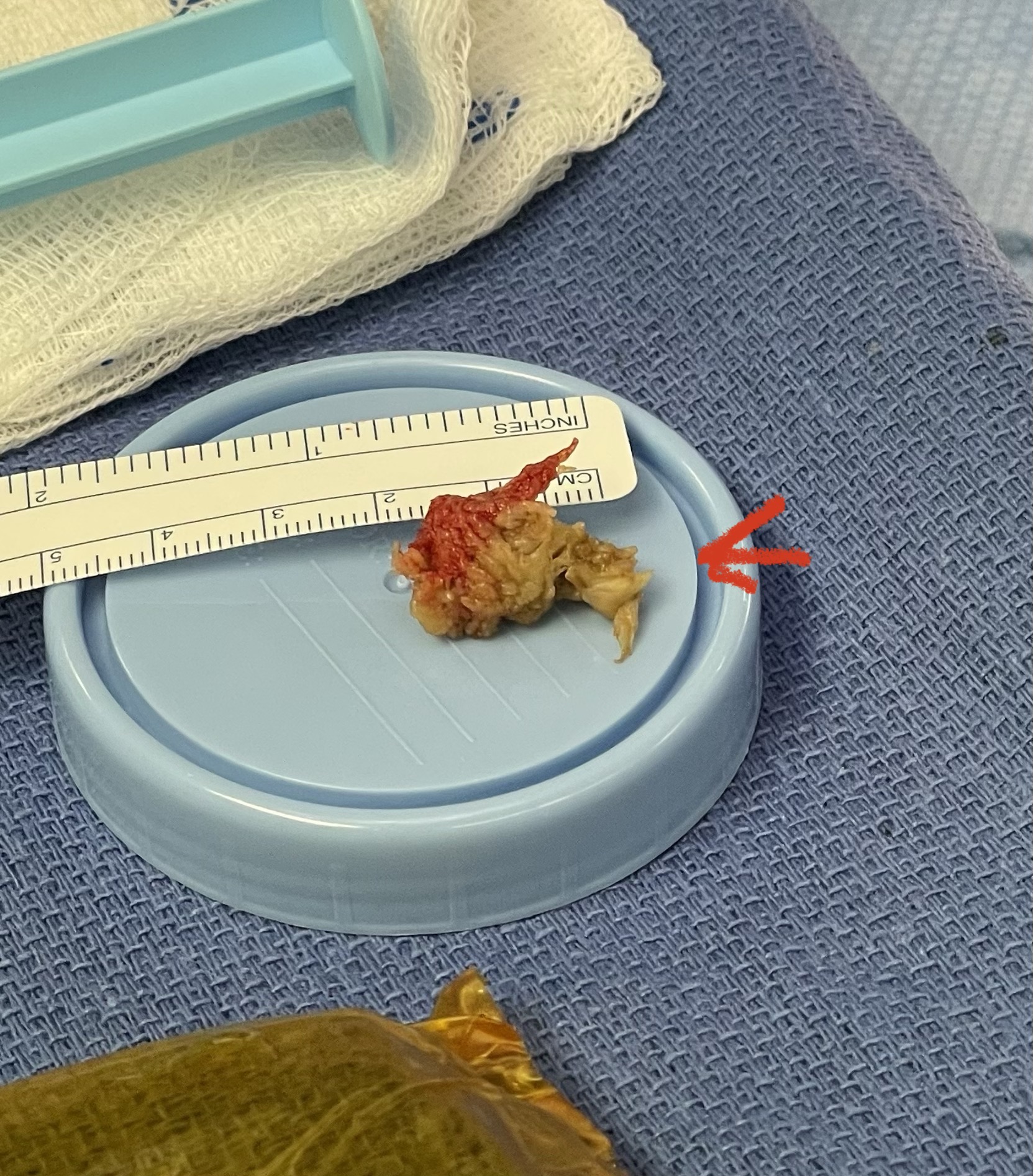
Fig 1: Upbiting curette
Revision lumbar spine surgery is amongst the most difficult of surgeries, not just in spine surgery, but of all categories of surgery. I don’t believe many spine surgeons will argue with this fact. The placement of hardware is getting slicker and easier, but there is no modern computerized technology that will improve upon the ability to separate and pick away scar tissue to establish dural planes in order to successfully decompress a patient who has redeveloped stenosis after a prior laminectomy and fusion. It does in fact take time and experience to understand what you can and can’t get away with, with regards to pressure, tension, aggressiveness of separation of planes during a dissection, and how to use the necessary tools to your advantage. A very important tool is the upbiting curette (Fig 1), which allows bone to be separated from soft material like scarred dura. This requires a very close hugging action to the undersurface of the bone of the lateral recess; if you get comfortable you can sweep an opening plane between the bone and dura since the back edge of the curette is smooth. It is important to identify opportunities of separation of planes and being patient to tend to a certain region first in order to gain the necessary plane to help you tackle another region that would have been difficult from an initial approach.

Fig 2: Kerrison device
Other maneuvers are always having a ready feeling of letting go of the tissue, having a light touch like “pumping your brakes”. Also, it is sometimes necessary to “shovel” the tissue, not bite it, with the Kerrison (Fig 2), utilizing the device as a dissecting instrument as well. It is also important to be patient and take the tissue in two bites, if necessary. It is ok to bite thickened tissue incompletely with the Kerrison if one is not sure if the consequence would be a leak or tear in the membrane if adhesions are present; dissect the adhesion with a Penfield 4 and cut it with a Metzenbaum scissors and then proceed with the finishing bite. The older patients are particularly challenging given the quality of their dura; it is often quite thin and floppy. A useful technique is employing an ultrasonic device (Fig 3) to remove enough of a shelf of bone to gain a dissection plane to allow for Kerrison to take over. And one can start with a 1 or 2 mm Kerrison to make a start under the edge of the bone and compressive soft tissue and advance to a 3 or 4mm.

Fig 3: Demonstrating the Misonix ultrasonic emulsifier to safely remove bone without injuring the dura and soft tissues.
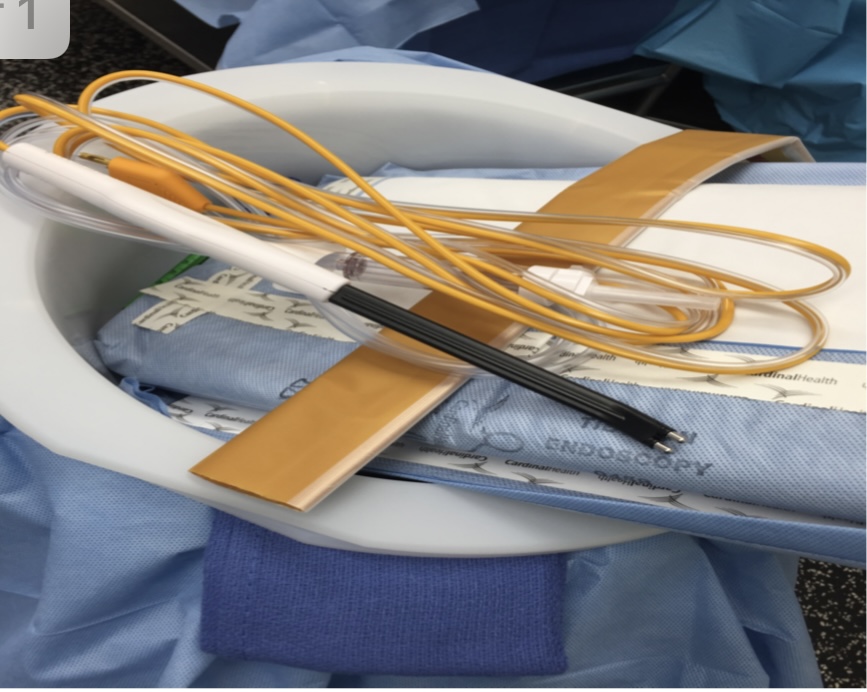
Fig 4: Aquamantys transcollation device for wide hemostatsis during revision lumbar surgery.
Another challenge in revision surgery is hypervascularity from scarring. In order to minimize excessive bleeding from exposure a very revolutionary tool is the Aquamantys transcollation device (Fig 4). It looks like a large bipolar with wider, thicker tips where instead of using electrocautery it uses saline and radio frequency to “shrink” not burn the blood vessels, utilizing less heat. This allows a larger swath of tissue to be covered to achieve hemostasis without having to precisely coagulate each blood vessel. This saves quite a bit of time and decreases blood loss considerably.
In cases where an instrumented fusion is done, you can freely remove the facet complex in order to gain a lateral position to the dural plane. Since you are fusing across the segment, you may take the inferior process of the lamina with impunity. This allows lateral access to the descending nerve root and the foramen. If a patient with a prior L5-S1 instrumented fusion develops next segment stenosis and degeneration at L4-5, an important first move is to define the inferior L4 lamina edge and the lower tips of the inferior facet processes. By removing the upper screw from the prior construct, this allows this maneuver more easily. Once you define the joint space you can remove the inferior facets with the combination of the curette and Kerrisons and bite the processes away to allow a dissection plane laterally along the dural edge, and with the Kerrison, define and decompress the foramina of the exiting L5 nerve roots. Often the Kerrison by feel, despite the scarring, can dissect through the plane to allow you to perform the foraminotomy starting under the lip of the superior lateral lamina, medial to the superior facet process of L5. If the prior construct is solidly fused then one can remove the L5 and S1 screws, add two new screws at L4 and at L5, leaving the S1 screws out and fusing L4 to L5, keeping a short segment construct.
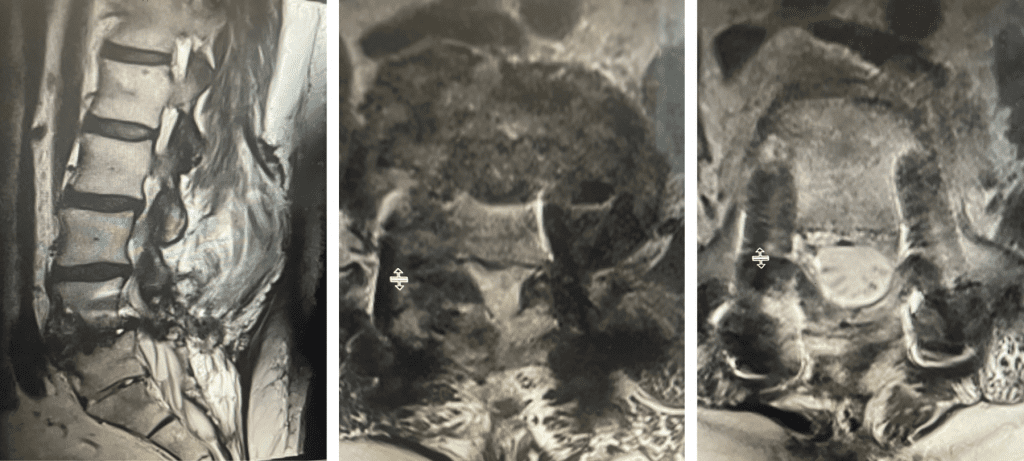
Fig 5a and b: T2-weighted sagittal and axial MRI demonstrating recurrent stenosis and instability after pseudoarthrosis of the L4-5 level. Note axial image showing normal canal diameter below L5.
Here is an example of an interesting case of a 54-year-old male who had had an L5-S1 laminectomy and fusion with instrumentation. At that time, our team had used BMP as an adjunct to bone graft for his fusion. This material is a hormone that is soaked in a resorbable sponge that helps induce bony fusion. He had done well and went on to have a solid radiographic fusion. The patient subsequently had developed a carcinoid tumor of the appendix for which he was treated. Four years after the patient was treated for the cancer, he developed next segment degeneration and stenosis and had revision surgery at L4-5 with instrumentation. Because BMP is not used in cases with a history of cancer since it is a growth factor, it was not used. The patient did well initially but subsequently over the last year developed severe progressive pain in his legs with numbness as well as low back pain. Imaging revealed the development of a spondylolisthesis at L4-5 with severe stenosis (Fig 5).
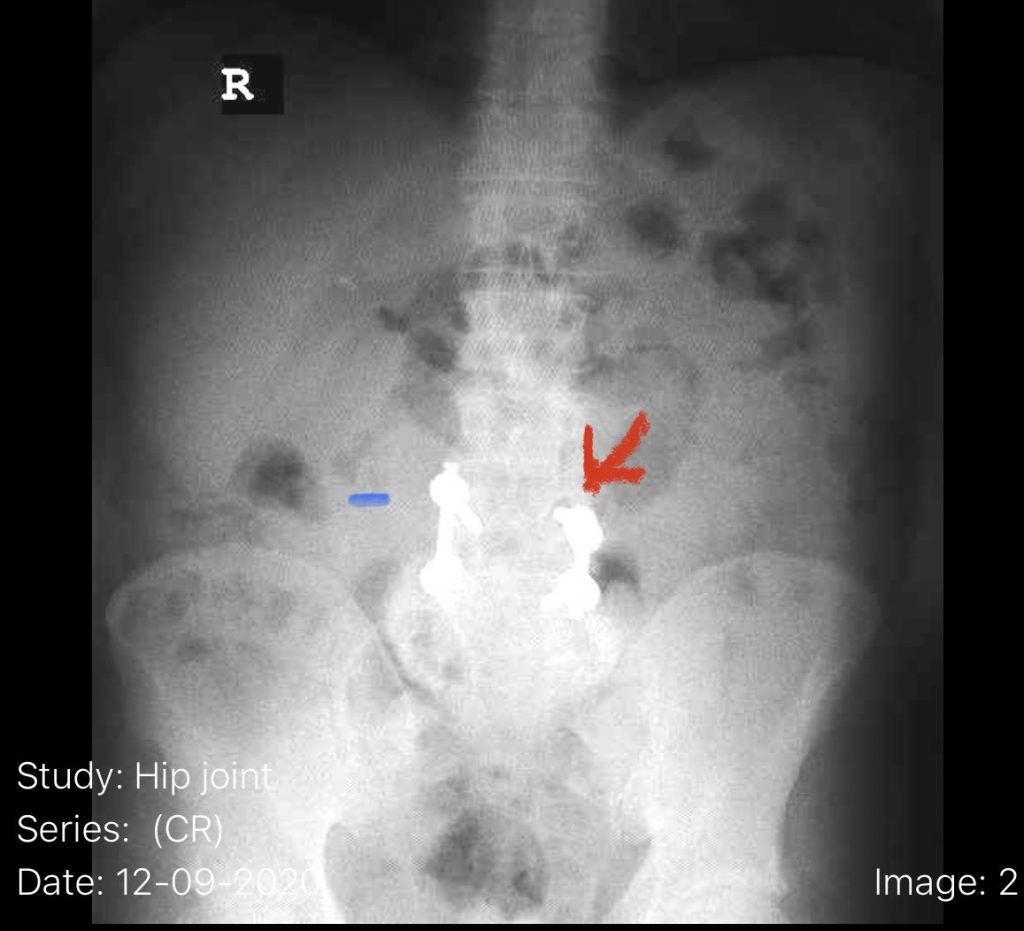
Fig 6: Plain AP x-ray demonstrating a lucency around the L4 screw (red arrow). Note the paucity of bone at the L4-5 level (blue dash) compared to below at L5.
The patient also had a retrolisthesis at L3-4 with mild stenosis. It was also noted that he had lucencies around the L4 screws, suggesting a pseudoarthrosis at L4-5. which is a lack of bony fusion (Fig 6). Patient was had failed conservative management and was taken to the operating room where his construct was explored. There was a complete lack of bony fusion mass between L4 and L5 and the screws were loose. Interestingly the L5-S1 region had a solid bony fusion where we had used BMP, but the L4-5 region did not. We removed the construct and removed the remnant of L4 lamina and the inferior processes and decompressed from L3 to to L5, decompressing well the L4 and L5 nerve roots. We placed new instrumentation from L3-5 with the use of BMP which was discussed with the patient prior to surgery (Fig 7). We also felt it was necessary because of the failure of the fusion. Post operatively the patient had an uneventful course with significant improvement of his prior symptoms.

Fig 7: Intraoperative fluoroscopic AP image of the new construct from L3-5. Note the very large lucency around prior L4 screw



