- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
SOMETIMES YOU HAVE TO CONNECT THE SKULL TO THE NECK
Adult Brain Surgery Spring 2024 Newsletter
May 9, 2024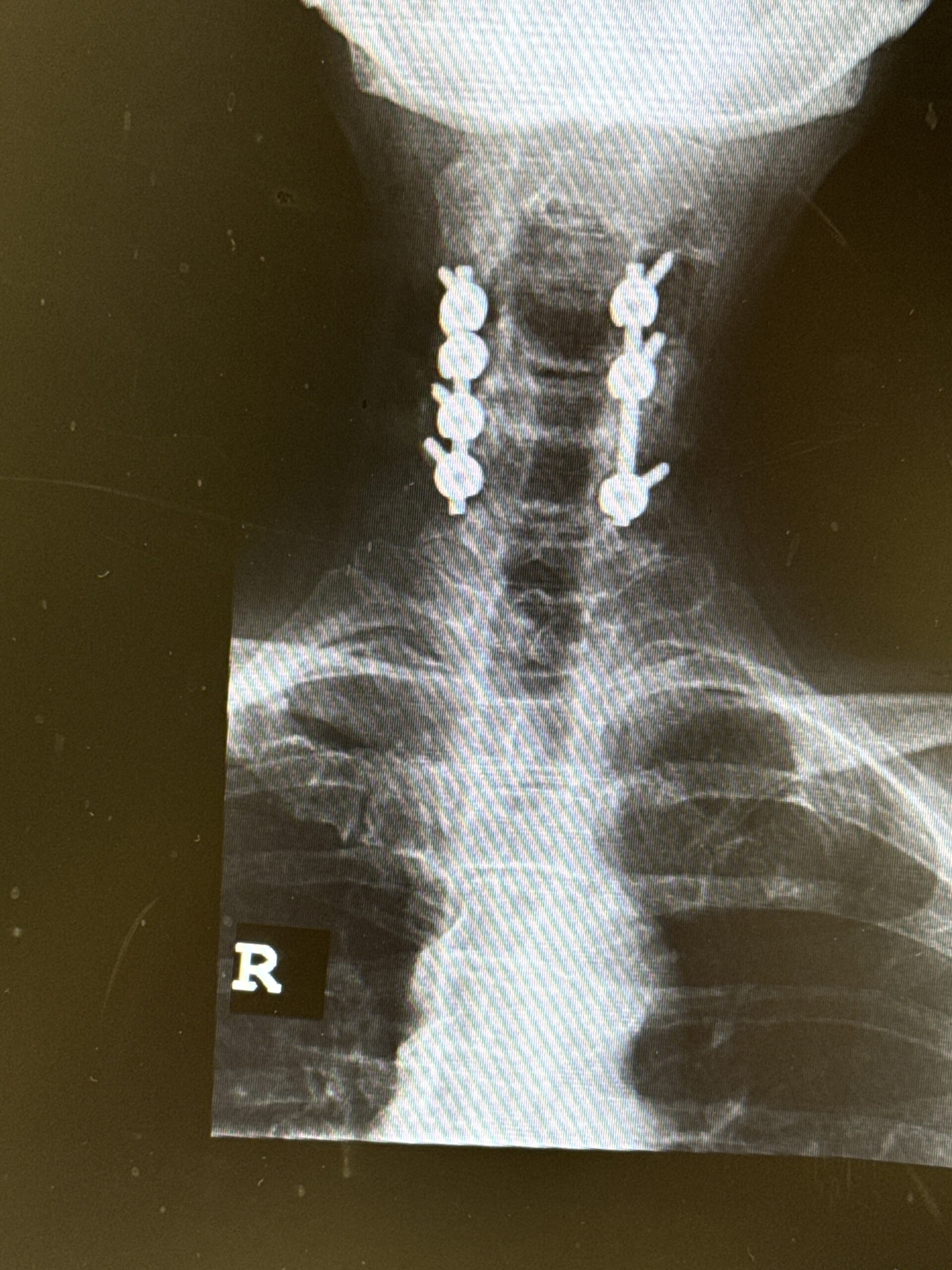
IMPORTANT CONSIDERATIONS IN SPINE SURGERY
August 27, 2024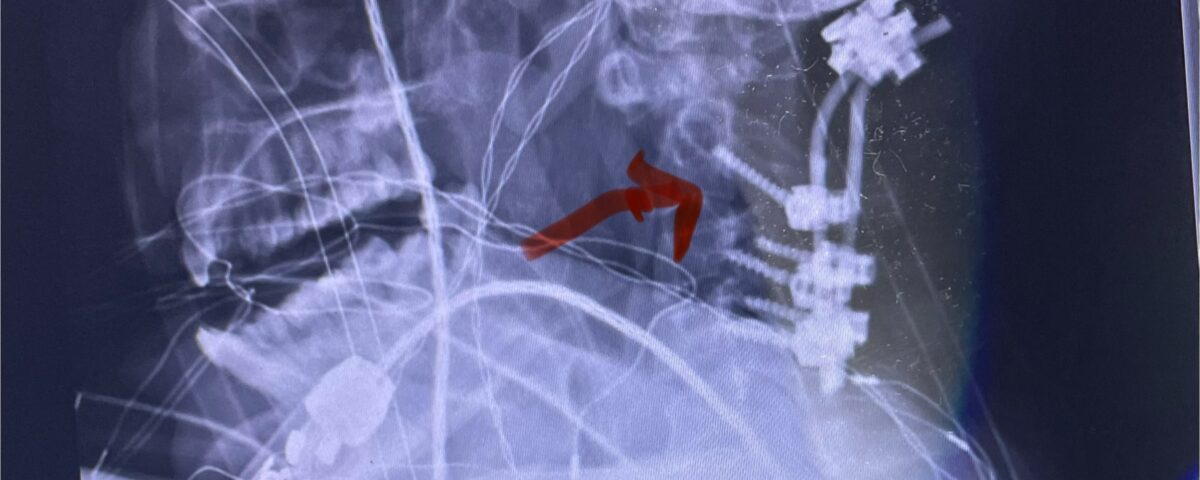
Fig 8: Intraoperative photograph demonstrating occipital-cervical construct and C1 laminectomy (blue dot). Note the 3 screws in the midline keel (blue arrow)
Patients may require an occipital-cervical fusion for both cranio-cervical and atlanto-axial instability, depending on the anatomy. Patients who have long segment posterior cervical fusions can sometimes develop next segment degeneration and instability as well, particularly at the C2-3 junction. They may require this procedure with settling of the skull base articulation with the cervical spine often with a resultant anterior odontoid pannus formation and spinal cord compression, particularly in those patients with rheumatoid arthritis. Certain select patients with Chiari malformations who have had a prior suboccipital craniectomy and upper cervical laminectomy may develop subsequent instability and require an occipital-cervical fusion.
This operation is a fairly extensive procedure and is a big deal for a patient to fuse their skull to the cervical spine, but sometimes it is necessary to prevent significant pain and neurological injury. The patient is positioned similar to a posterior cervical procedure but one must expose the subocciput to the inion. Oftentimes there are cranial-cervical congenital abnormalities at the craniocervical junction that the surgeon must be aware of prior to surgery. Therefore, it is critical to have a complete analysis of the cranial cervical anatomy with MRI and fine-cut CT scan preoperatively. It is imperative that at the upper cervical spinal levels particularly at C1 and C2 during a decompressive laminectomy one is so careful regarding any downward pressure on the spinal cord and lower brainstem at the level of the foramen magnum. A good number of these patients have myelomalacia indicating chronic compression and instability. In my experience the use of a diamond burr to thin the lamina to make it much easier to flake away and decompress the spinal cord with a fine Kerrison and curette. Another useful device is to use the Misonix ultrasonic bone emulsifier to essentially “melt” the bone away without affecting the soft tissue such as the dura. This device requires no downward pressure.
Although some patients do not require a decompression and just require an occipital cervical fusion, most require some sort of decompression of the neural elements. After a decompression an instrumented fusion is performed. A useful anatomic structure for anchoring the top portion of the construct to the skull is the midline keel of the subocciput. This structure extends from the external occipital protuberance, which corresponds to the confluence of the sagittal and transverse sinuses, to just above the foramen magnum:
(Fig. 1). This bone is quite thick, about 15 mm (Figs. 2a and b). Most modern plate systems utilize three midline keel screws with the option to place within a 2 cm lateral fixation point. This plate is connected to sometimes tricky-to-bend rods and connected to screw fixation points in the cervical spine (Fig. 3). Bone graft material extends from skull to cervical spine.
Here are some illustrative cases where we felt it was necessary to perform an occipital-cervical fusion:
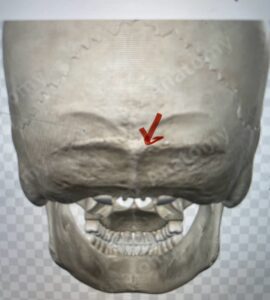
Fig. 1: Diagram of occipital bone to foramen magnum. Note external occipital protuberance (red arrow)
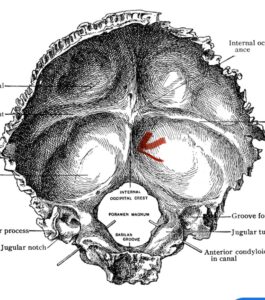
Fig. 2a: Cartoon illustrating posterior projection of internal skull structures demonstrating the midline keel in the subocciput above the foramen magnum.
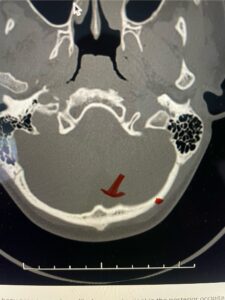
Fig. 2b: Axial CT scan of the brain demonstrating the thickness of the midline keel (red arrow) compared to the more lateral subocciput (red dot) making the keel ideal place for screw fixation
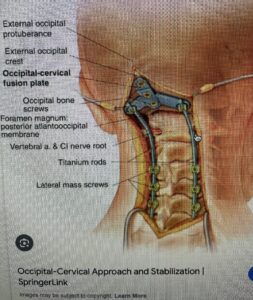
Fig. 3: Cartoon demonstrating an occipital-cervical construct utilizing the midline keel for fixation
This is a 42 year-old female who presents with severe progressive weakness and numbness and difficulty with balance over a 6-month period. She has a history of having a motor vehicle accident at 5 years old but was never imaged. On exam she was noted to be severely myelopathic. Imaging revealed severe spinal cord compression at the level of C1 (Figs 4a and b).
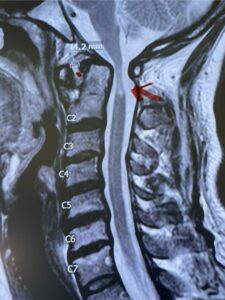
Fig. 4a: Sagittal T2-weighted cervical MRI demonstrating severe cord compression with myelomalacia of upper cervical spinal cord (red arrow). Notice the increased atlanto-dens interval (red dot).
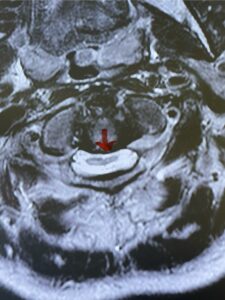
Fig. 4b: Axial T2-weighted cervical MRI demonstrating severe spinal cord compression from atlanto-axial instability (red arrow)
Cervical x-rays revealed a significantly increased atlanto-axial interval (Fig. 5) On review of her imaging studies it was noted that the right C2 isthmus was very thinned by the vertebral foramen (Figs 6a, b, and c) which would make an attempt at placing a C2 pars screw dangerous. A decision was made to perform an occipital-cervical fusion because only possible unilateral fixation and an extensive C1 laminectomy to be performed eliminating a fixation point if a more traditional C1-C2 was performed. Even if C1 lateral mass screws were able to be placed one could only perform a unilateral screw construct fixation to C2. We performed an occipital cervical fusion down to C4 to get enough inferior fixation and C1 laminectomy. The decompression went well. We placed a left unilateral pars screw and bilateral C3 and C4 lateral mass screws. We placed three 12 mm screws in the midline keel (Fig. 7). Postoperatively the patient had all around improvement in her symptoms and did not qualify for rehab. Her post op films at 6 weeks (Fig. 8)
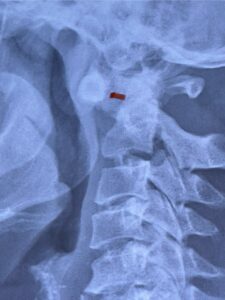
Fig. 5: Lateral cervical x-ray demonstrating widened atlanto-dens interval as a result of instability (red dash).

Fig. 6a: Sagittal cervical CT scan demonstrating an abnormally thin right C2 isthmus prohibiting safe placement of screw (red arrow). Notice the vertebral foramen eroding the isthmus bone structure (red dot).

Fig. 6b: Sagittal cervical CT scan demonstrating normal thickness of the left C2 isthmus (red arrow)
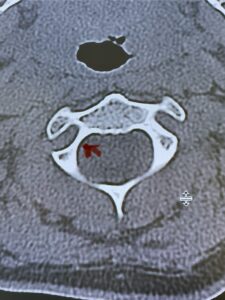
Fig. 6c: Axial cervical CT scan demonstrating a very thin right C2 isthmus (red arrow) compared to left side.

Fig. 7: Intraoperative photograph demonstrating occipital-cervical construct and C1 laminectomy (blue dot). Note the 3 screws in the midline keel (blue arrow)

Fig. 8: Intraoperative photograph demonstrating occipital-cervical construct and C1 laminectomy (blue dot). Note the 3 screws in the midline keel (blue arrow)
This is a 59 year-old female with a history of cerebral palsy and a prior C3-C7 posterior cervical laminectomy and instrumented fusion two years prior. She did ok until she developed progressive weakness of all four extremities and numbness. Imaging revealed she had a significant breakdown above the fusion at C2-3 with a grade 2-3 spondylolisthesis of C2 on C3 with severe spinal cord compression (Fig. 9). It was surprising the degree of anterior fusion induced by the posterior fusion from C 3-C 7 (Fig. 10). Because of her progressive neurological dysfunction in a patient who was already compromised because of her cerebral palsy, it was clearly necessary to decompress from occiput to C 3. We utilized her prior lateral mass screws although we removed bilaterally the C7 screws to reduce the fulcrum-effect on the C7-T1 junction as the C 6-7 level was solidly fused. We performed an occiput to C 6 fusion with occiput to C3 laminectomy (Fig. 11) Post operatively we had good placement and alignment (Fig. 12) The patient went to rehab with improvement of strength and numbness particularly in hands.

Fig. 9: Sagittal T2-weighted cervical MRI demonstrating severe upper cervical spinal cord compression secondary to C2 anterior subluxation on C3 with development of thickened posterior degenerative material (red arrow).

Fig. 10: Sagittal cervical CT scan demonstrating grade 2-3 subluxation of C2 on C3 above prior C3 to C7 posterior instrumented fusion and laminectomy (red arrow). Note the unusual significant anterior auto fusion resulting from prior posterior construct (red dot).

Fig. 11: Intaoperative photograph demonstrating an occipital-cervical construct and occipital to C3 laminectomy. The blue material is a fibrin sealent over the laminectomy defect
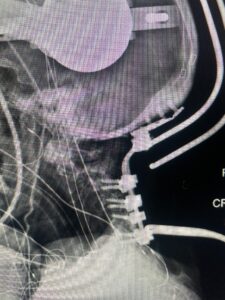
Fig. 12: Intraoperative lateral X-ray demonstrating good placement of occipital-cervical construct



