- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Thoracic Stenosis
Cysts
July 2, 2022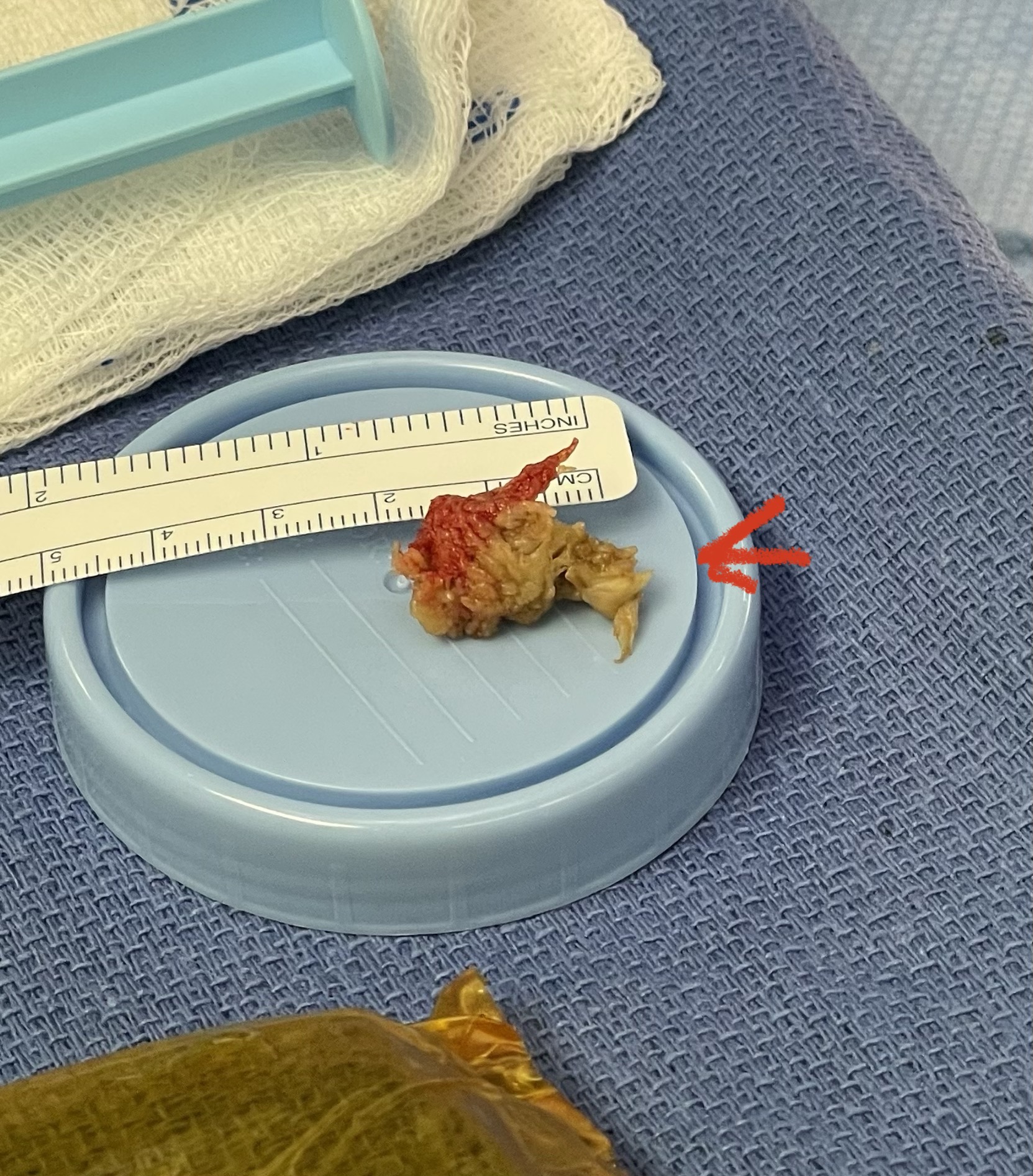
Lateral Disc Herniations
August 23, 2022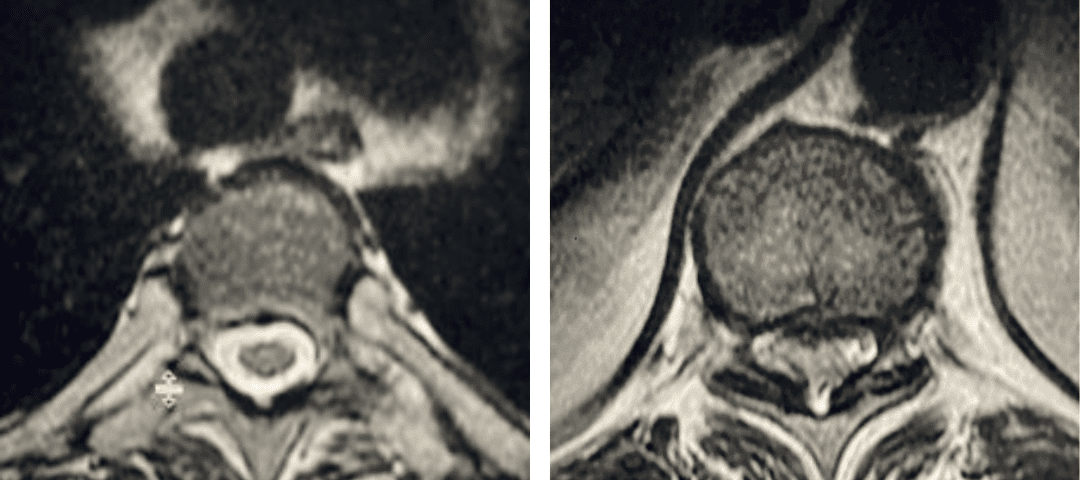
fig 2 thoracic
Thoracic stenosis is far less common than lumbar stenosis. Whereas the symptoms of lumbar stenosis are usually well-defined, thoracic stenosis can act like a great mimicker, and often presents with a myriad of symptoms and signs. Thoracic stenosis is scary as are the symptoms which include progressive weakness either unilaterally or bilaterally, foot drop, difficulty walking, proprioceptive dysfunction, and bowel and bladder dysfunction. Patients don’t always present with pain in the back or legs. They can have numbness. Patients can also have concurrent lumbar stenosis. However, the weakness in thoracic stenosis tends to be more common proximally in the legs with perhaps upper motor signs. In the lumbar spine patients will tend to more commonly have lower lumbar disease with pain down the leg below the knee and tend to have minimal neurological deficit. The spinal cord is in play throughout the thoracic spine as compared to the lumbar spine whereas the spinal cord is only involved at the uppermost lumbar segment. The thoracic spinal cord is far less forgiving and has a tenuous blood supply. In the lumbar spinal canal, there can be severe circumferential stenosis of the lumbar thecal sac before ANY symptoms or neurological deficit occurs. In the thoracic spinal canal because of the tenuous blood supply of the spinal cord, compression of the spinal cord can result in more severe deficit and certainly with the same degree of stenosis as lumbar can cause much more severe symptoms and neurological deficit.
The thoracic spine is supported by the rib cage which provides stability and support. There is a lack of motion and hence a reduced incidence of formation of compensatory arthritis. This development of arthritic structures includes ossification and thickening of the posterior ligament, facet hypertrophy, herniated calcified disc or anterior osteophyte. Thoracic stenosis more commonly occurs in the lower thoracic segments although this may occur as well in the upper thoracic spine. This may be determined by body habitus and weight. Long term compression of the spinal cord can result in myelomalacia or signal change in the spinal cord on MRI indicating long term compression and potential irreversible damage. Early intervention for myelopathic signs is imperative and operative. There is more leeway with symptoms and signs of lumbar stenosis to treat conservatively and nonoperatively as most patients present with no neurological deficit.
Thoracic stenosis with cord compression is generally operated on by a posterior thoracic laminectomy and decompression. It is rare that a patient has a massive, calcified disc herniation causing solely anterior spinal cord compression. In those circumstances anterior and anterolateral approaches may be considered. As is during a posterior cervical laminectomy a decompression should extend well above and below the pathology to allow the bowstring effect or prevent constricted decompression, allowing the spinal cord to drift posteriorly from the ventral spinal pathology. The decompression must be delicate to put the least pressure on the cord; the motion vector of the decompression should be sliding and lateral with minimal ventral pressure. Depending on the degree of facet joint removal, degree of kyphosis, and prior training will dictate a surgeon’s decision to augment the decompression with a fusion with or without instrumentation.
Postoperative outcome is dependent on the patient’s preoperative condition and degree of neurological deficit. Certainly, patients with evidence on MRI of myelomalacia may have a slower recovery with a less certain outcome. In any surgery for patients with spinal cord compression the most important reason for the surgery is to prevent the patient from getting worse and preserve neurological function. However, if the surgery is well indicated and because this is a benign disease, patients as a rule improve but to the extent, they do is uncertain as we are dealing with the central nervous as in the brain and spinal cord, and not a peripheral nerve as in the case in the lumbar region. Here is a case that illustrates what can evolve in terms of neurological decline with thoracic stenosis in a particularly challenging patient because of her morbid obesity.
Case Study:
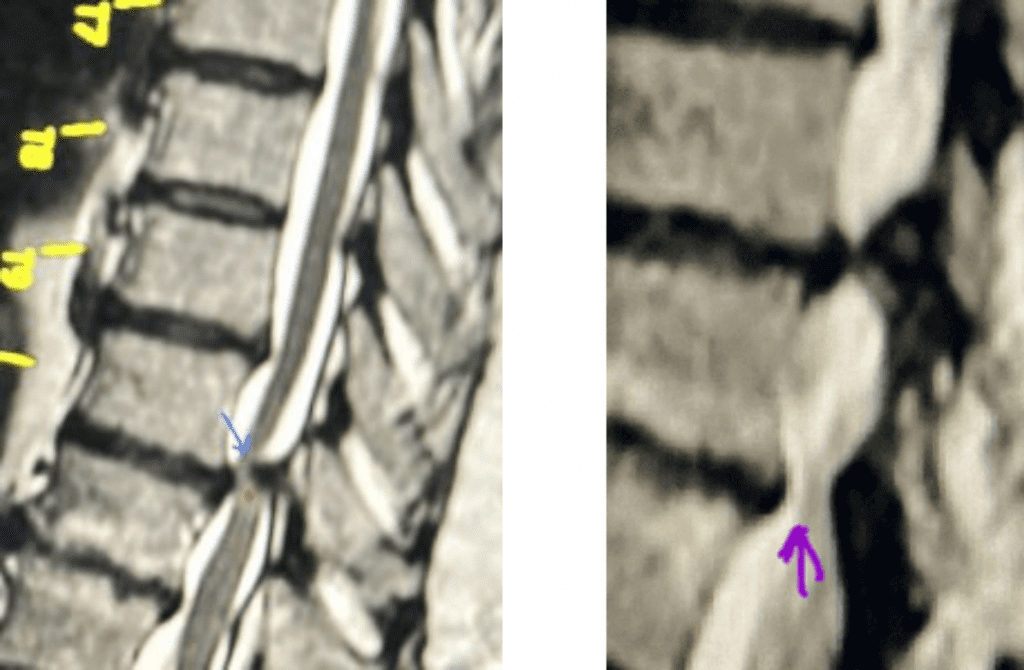
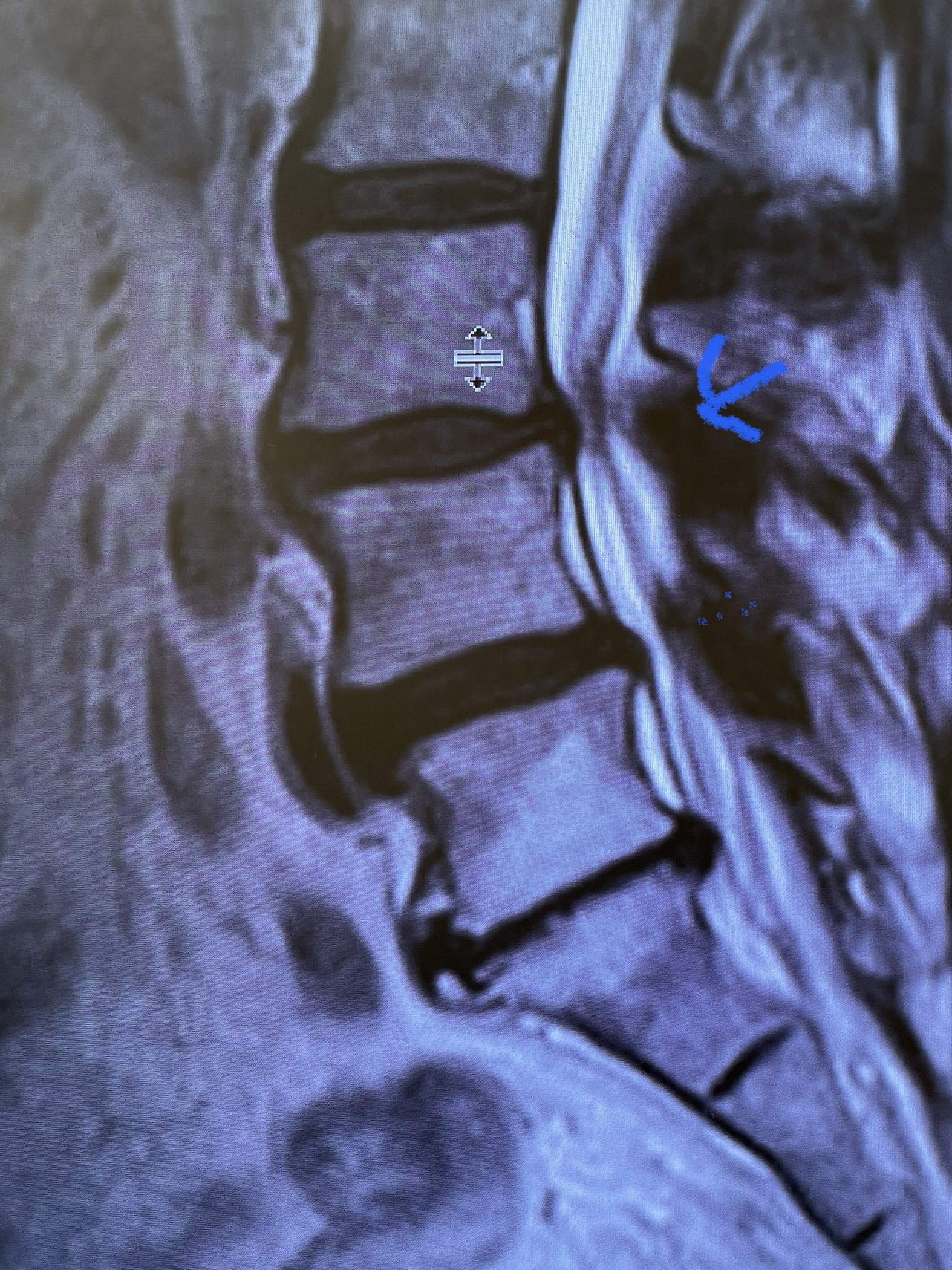
Figure 1. The sagittal MRIs demonstrate a very tight stenosis at T10-11 (blue arrow). Note the area of hyperintensity within the spinal cord at this level representing myelomalacia (red dot). Patient also has significant stenosis at T11-12 (purple arrow).
This 50-year-old morbidly obese female presents with one month of progressive weakness of her lower extremities. She also reported numbness and pain in her thighs. Her right leg was worse, and she had one episode of urinary incontinence. She had some back pain. She was ⅖ strength in her right hip flexor and quadriceps. She was ⅘ in her left lower extremity. MRI (Figure 1 and Figure 2) revealed very tight stenosis circumferentially at T10-11 secondary to facet hypertrophy and anterior disc osteophyte complex with associated myelomalacia of the spinal cord. There was also stenosis to a lesser degree but still significant at the T11-12 level.
It was felt given her severe, progressive neurological deficit to proceed with an urgent decompression from T9-T12. Given the patients age, obesity, necessary wide laminectomy requiring partial facet removal, and proximity to thoraco-lumbar junction we also augmented her laminectomy with an onlay fusion or in situ fusion. Because the patient had a fairly minimal kyphosis and had severe degenerative disc space narrowing, we did not feel it was necessary to add instrumentation to her fusion.
Intraoperatively as expected it was extremely tenuous as the spinal cord was very compressed necessitating us to be quite cautious during each move to remove the arthritic material of the overgrown facet and ligament with our kerrisons and curettes. Post operatively the patient had a dramatic improvement in the recovery room of her strength and was discharged home about a week later. This was a case that was very satisfying for us as surgeons.
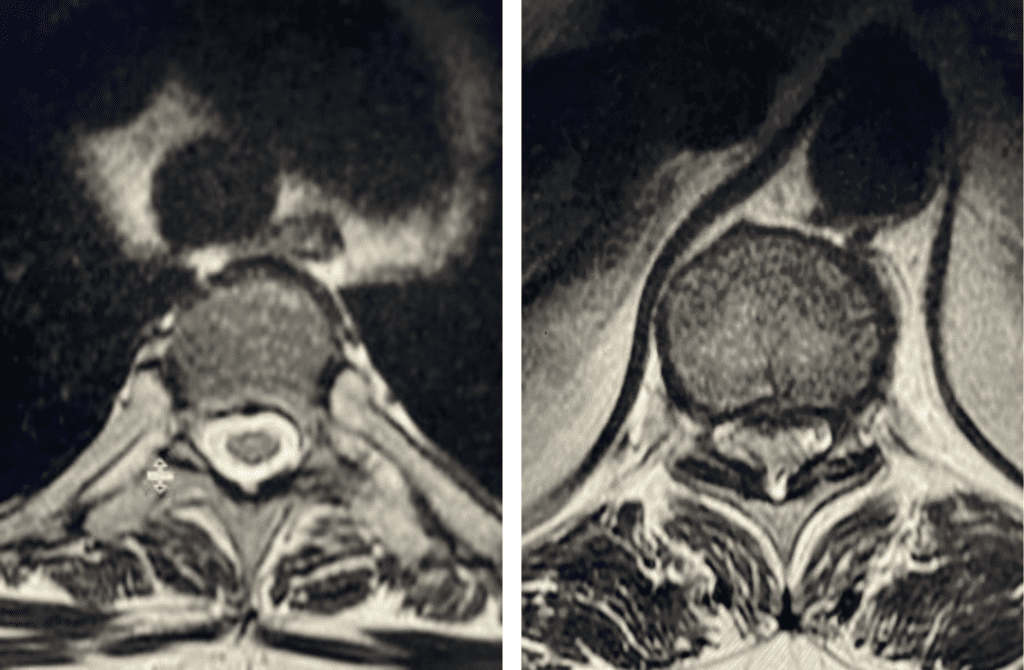
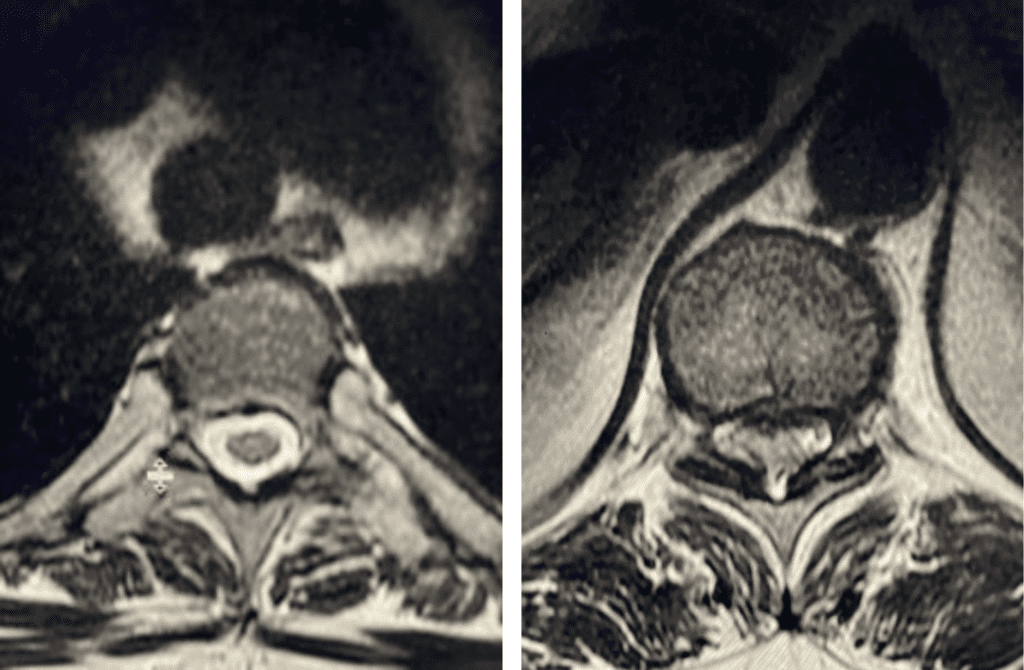
Figure 2. Axial images comparing a normal appearing spinal cord with a white fluid ring around it versus an axial image of the T10-11 level demonstrating circumferential stenosis.