- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Spine Cases Where Surgery Is Clearly Indicated
Watch how a thoracic laminectomy allows for successful removal of a spinal cord mass
August 16, 2023NSPC Neurosurgeon Dr. Michael Brisman Authors Brain Surgery Textbook
January 4, 2024
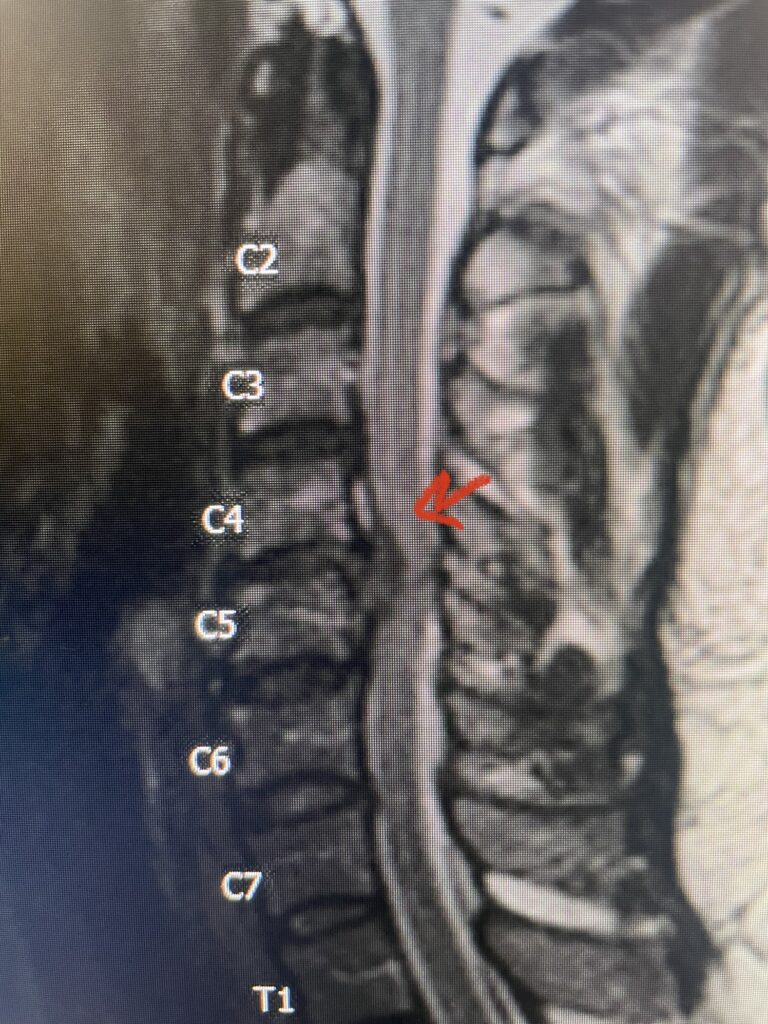
Fig 2a Sagittal and axial T2 weighted cervical MRIs demonstrating large C4 5 herniated disc with spinal cord compression red arrows
One of the more interesting aspects of neurosurgery is making a decision as to whether a patient should have spine surgery. If a patient has severe spinal cord compression from a compressive lesion such as a herniated disc and a progressive spinal cord dysfunction or myelopathy, then surgery is indicated to relieve the compression.
Patients with cervical or thoracic myelopathy or signs of spinal cord compression have a more serious condition than a patient that has pain from a peripheral nerve being compressed in the cervical spine or lumbar region. In a patient with signs of cervical myelopathy with progressive loss of function, surgery is generally indicated and supersedes injections and physical therapy, unless the patient cannot tolerate surgery or have minimal symptoms.
Patients with lumbar stenosis, for example, anatomically may have severe lumbar spinal canal compression from thickened ligamentum hypertrophy and facet arthropathy, but most only present with back pain and a mild neurological deficit or no deficit at all. This is because the compression develops so slowly the peripheral nerves of the thecal sac are able to accommodate this compression. Most patients don’t know that the spinal cord ends at L1 so that in the lumbar canal we are only dealing with the peripheral nervous system versus the spinal cord which is the central nervous system is much less forgiving.
Therefore, in the management of a patient with a “pinched nerve” there is more leeway. Oftentimes in these patients pain as well as neurological deficit will resolve with conservative management such as physical therapy, injections by pain management, and most importantly the tincture of time. Patients, however, who do have a compressive lesion of their nerve whether it be a soft herniated disc or spondylitis change such an osteophyte or thickened ligament and fail conservative management can be indicated for surgery.
Patients who have surgery for myelopathy the most important reason is to prevent the patient from getting worse. Because you are dealing with the central nervous system, the extent of return of neurological function is not always known although properly indicated cases can have dramatic improvement even in the recovery room. The following cases illustrate these points and in my opinion are surgically indicated:
This 67-year-old female presents with progressive heaviness and numbness of the legs and difficulty ambulating. Her right leg was worse than her left. She had right greater than left hip flexor weakness. She was hyperreflexia in her lower extremities. An MRI (Fig. 1) demonstrated an intradural arachnoid cyst at T10-11 with severe spinal cord compression. She also appeared to have an arachnoid cyst above from T4-T8 with anterior displacement and compression of the spinal cord. Because of her severe myelopathy and the findings on MRI the patient underwent laminectomy for surgical decompression of cyst. Intraoperatively the focal arachnoid cyst at T10-11 appeared as a small bubble crushing the spinal cord anteriorly with scarring of the arachnoid with no CSF flow above or below.
The cyst was fenestrated and immediately CSF flow was reestablished. We performed a laminectomy at T6-7 for the upper cyst region which was observed to be more consistent with normal anatomy. We fenestrated the arachnoid. It was felt that the upper level was a secondary phenomenon as a result of CSF flow blockage. Post operatively she had an uneventful course with return of normal strength although she had some residual numbness.

Fig. 1 Sagittal T2-weighted thoracic MRI demonstrating both T10-11 focal intradural arachnoid cyst (red arrow) and larger upper thoracic cyst that appears to extend from T4-T8 (blue arrow).
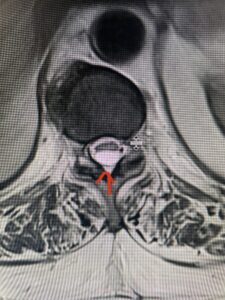
Fig. 1b Axial T2-weighted thoracic MRI demonstrating spinal cord compression from T10-11 arachnoid cyst (red arrow)
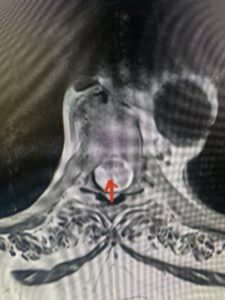
Fig. 1c Axial T2- weighted thoracic MRI demonstrating spinal cord compression with severe anterior displacement of the spinal cord from upper thoracic arachnoid cyst.
This 47-year-old male who four months prior was lifting weights developed sharp pain in his neck. After that he developed progressive numbness in his arms, neck pain and headache. He said that the right arm was worse than the left. On examination the patient had long tract weakness on the right side which included his triceps, finger extensors, hip flexors, and dorsiflexors. The patient did not have hyperreflexia. MRI (Fig. 2) demonstrated a massive, extruded disc herniation with severe cord compression. The patient because of progressive myelopathy and spinal cord compression was indicated for anterior cervical discectomy and fusion at C4-5 (Fig. 3). Patient had significant improvement of weakness and numbness post operatively.

Fig. 2a Sagittal T2-weighted cervical MRI demonstrating large C4-5 herniated disc with spinal cord compression (red arrow)
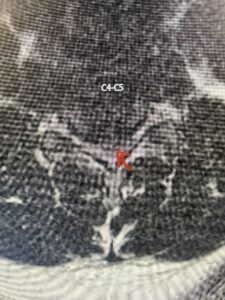
Fig: 2b Axial T2-weighted cervical MRI demonstrating spinal cord compression from C4-5 herniated disc (red arrow)

Fig. 3 Intraoperative lateral cervical X-Ray demonstrating C4-5 ACDF
This 36-year-old female who had a long history of neck pain had a history on MRI of a C5-6 bulge. She recently after diving into a pool (not hitting her head on bottom) developed progressive problems with her arms. She had developed spontaneous shocks going down her arms and in the back of her neck. Spontaneous shocks going down the neck and spine is called a Lhermitte’s phenomenon and can occur with spinal cord compression and also with multiple sclerosis. On examination, the patient had long tract weakness of her arms, right greater than left. Her finger extensor weakness was profound on the right. MRI (Fig. 4) of the cervical spine revealed a massive C5-6-disc herniation causing significant cord compression right greater than left with subtle cord signal change. Because of the severe myelopathy, the patient was indicated for surgery. A C5-6 anterior cervical discectomy and fusion was performed (Fig. 5). The patient had a dramatic improvement of her strength in the recovery room.

Fig 4. Axial T2-weighted MRIs demonstrating large C5-6 herniated disc with spinal cord compression (red arrow)

Fig 4A. Axial T2 weighted MRIs demonstrating large C5-6 herniated disc with spinal cord compression (red-arrow)

Fig 5. Intraoperative Lateral Cervical X-Ray demonstrating C5-6 ACDF