- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
YOU DON’T HAVE TO GET EVERY MORSEL
NSPC’s Fall 2024 Practice Journal
October 31, 2024
IT’S ALL ABOUT THE DECOMPRESSION…
March 3, 2025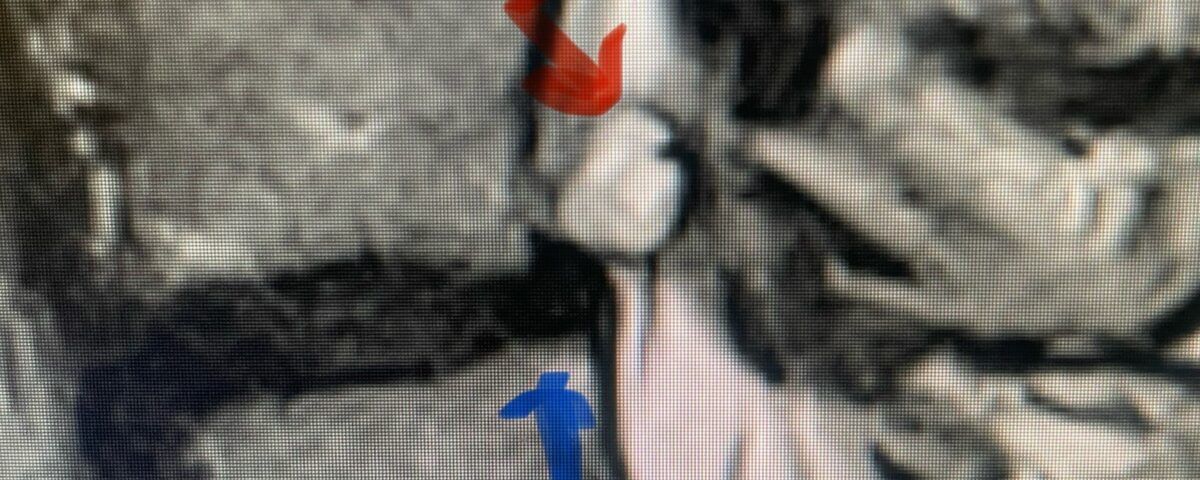
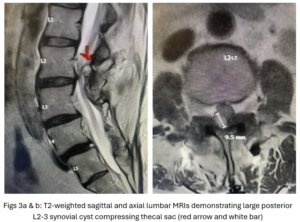
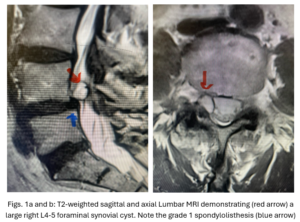
Figs 1a,b: T2-weighted sagittal and axial MRI demonstrating (red arrow) a large right L4-5 foraminal synovial cyst. Note the grade 1 spondylolisthesis (blue arrow)
The spinal synovial cyst is one of the most interesting expressions of spinal instability. They emanate from the synovial lining of a degenerated facet joint that will often be misaligned or diastatic. This extension forms from the synovial lining of the joint which will often assume a roundish structure. This cyst is often filled with jelly-like, necrotic material. There is sometimes fluid within these but in my experience, they are more filled with solid material. This accounts for often failed attempts at aspirating these. As a result of their formation and extension this can lead to serious compressive nerve root syndromes. In the lumbar spine, these cysts can be intra or extraspinal. The intraspinal cysts form posteriorly. When they extend from the facet joint, they often compress posterolaterally, which can involve both the foramen, thecal sac, or both. Interestingly, they can form almost completely posteriorly and appear to emanate from the lamina or ligamentum; but they always have some association with the medial facet complex. These will tend to cause spinal stenosis because of the degree of thecal sac compression.
Intraoperatively, these cysts will always form posterior to either the descending nerve root or the exiting nerve into the foramen because they must since the facet forms the posterior wall of the foramen. This is important in understanding anatomically where the nerve root will be which is anterior to the mass. There is often found to be inflammatory, thickened tissue over these structures and are commonly attached and even meld with the dura. The goal is to decompress the thecal sac and nerve root. In my experience it is unnecessary to remove 100 % of these masses as they are often stuck to the dura with risk of a resultant CSF leak. Of note during the dissection of these cysts there is often a release of cyst fluid and as result it can be alarming to the surgeon as one initially thinks it is CSF when in fact it is purely cyst fluid. The most important aspect is to internally decompress these masses. Although it is possible for these masses to reoccur, it is unlikely, particularly if a concurrent fusion is performed. By arresting the abnormal motion, the signal to make these formations is arrested. These cysts are really just a form of arthritis and in essence an aberrant attempt of the spine to stabilize itself.
CASE STUDY:
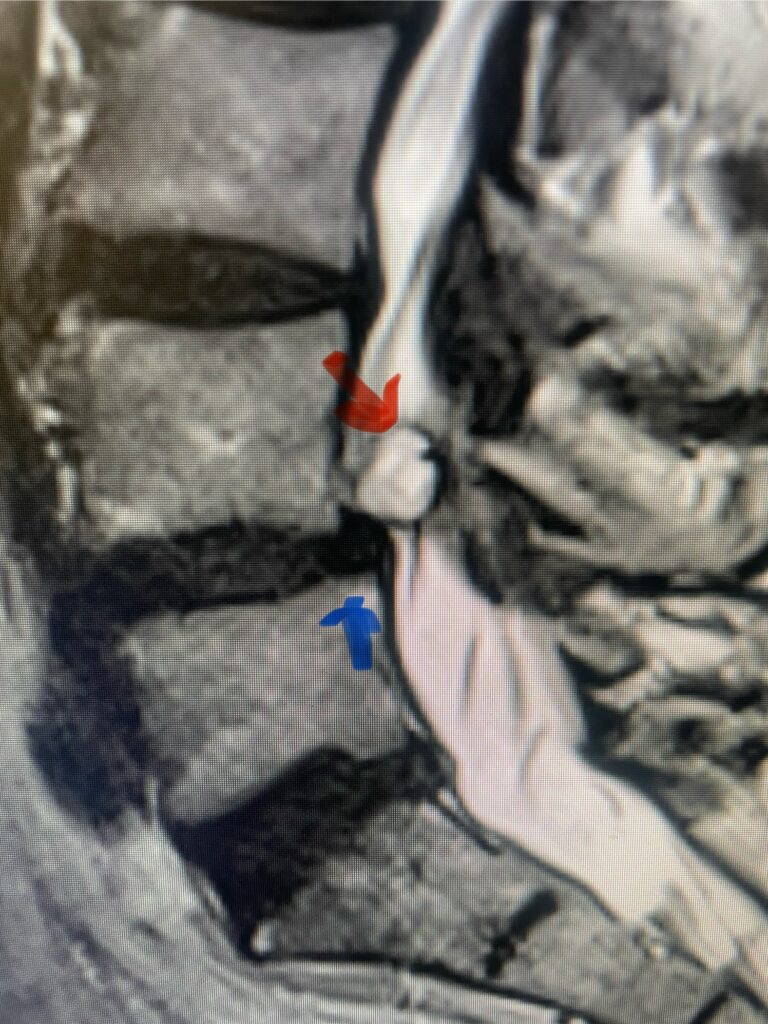
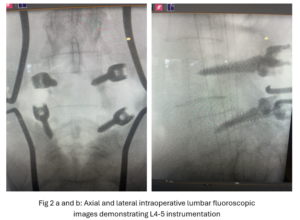
This 54-year-old female with a long history of low back pain presents with three weeks of a progressive right footdrop with associated numbness and tingling of the right leg. In addition, she had right lateral hip pain down to the dorsum of her foot. She first noticed her right foot slapping the floor when she walked. She had no prior trauma or unusual activity before this began. Her chiropractor, who had treated her back pain for a long time, first noticed the foot drop and referred her for further evaluation. She presented with ⅖ strength in her right dorsiflexor. MRI revealed a large right L4-5 foraminal synovial cyst with some mass-effect on the thecal sac. (Fig. 1) She also had an associated grade 1 spondylolisthesis. Because the cyst was more foraminally-oriented, it had the majority of its effect on the right L4 nerve root. It was felt the patient required surgery to attempt to reverse her weakness. We performed a decompressive laminectomy at L4, removing the inferior facet process on the right in order to gain lateral and foraminal access to the right L4 nerve root. In the lateral recess there was a heap of inflammatory tissue which we entered, revealing the cyst. The medial wall was stuck to the dura. We internally decompressed the cyst which was mainly gelatinous material with some fluid. We dissected and removed as much of the cyst we could safely remove but left the medial wall for fear of removing it would cause a CSF leak, upon removing the bulk of the cyst we encountered anteriorly the descending and exiting right L4 nerve root which was purplish in color and clearly inflamed. We performed a generous foraminotomy of the right L4 as well as the right L5 nerve root. We also performed an instrumented fusion at L4-5 (Fig. 2).
Postoperatively, the patient had a remarkable return to full strength of her right dorsiflexor within 24 hours. Her pain in the leg was also alleviated. She was discharged post op day 2.
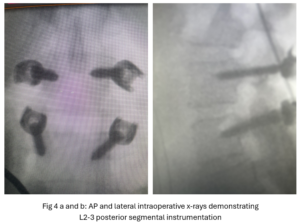
This 50-year-old female with a long history of low back pain and a prior history of multiple lumbar surgeries with instrumentation. She had a L3-5 laminectomy with instrumentation about 7 years prior and now presents with progressive worsening of low back pain. The pain was worse with activity, standing, walking, and prolonged sitting. She had an MRI which showed next segment degeneration at L2-3 with stenosis and the development of a large posteriorly-oriented synovial cyst with thecal sac compression (Fig. 3). The patient failed all means of conservative management including physical therapy and epidurals. We decided to perform an L revision laminectomy to decompress and remove the cyst as well as explore her prior fusion. In this case, again the anterior wall of the sac was completely stuck to the dural membrane. Therefore, we internally decompressed the cyst which was mainly degenerated, necrotic material and removed as much wall of the cyst that could be safely removed. There was some fluid within the cyst. Of note during the dissection of these cysts there is often a release of cyst fluid the patient was well-decompressed. We removed the prior instrumentation and added a new L2-3 construct (Fig. 4). The patient had an uneventful hospital course and was discharged on post op day 2.