- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Grade 1 Spondylolisthesis At L4-5 With Severe Lumbar Stenosis
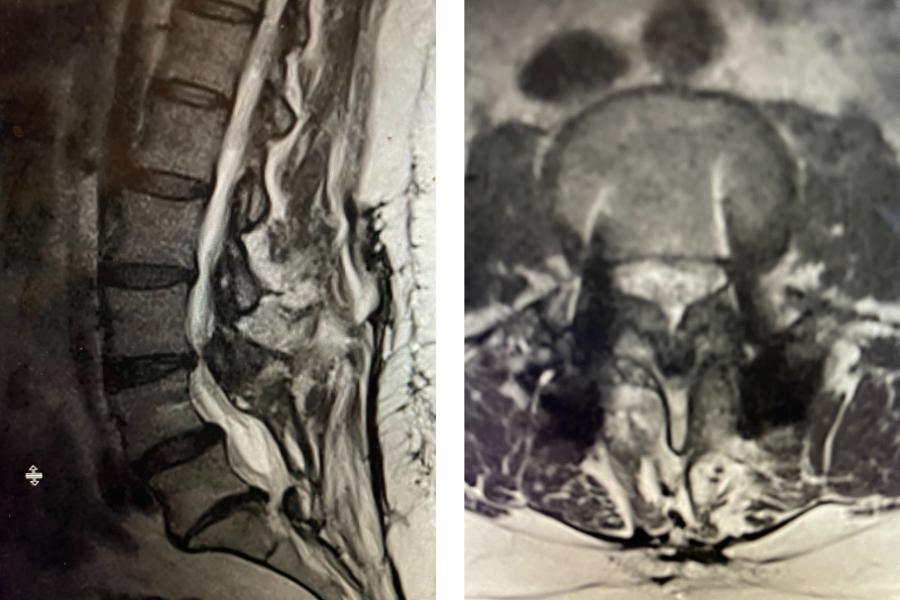
Severe Stenosis Above Prior Fusion
May 6, 2022
NSPC Mobile Patient
May 10, 2022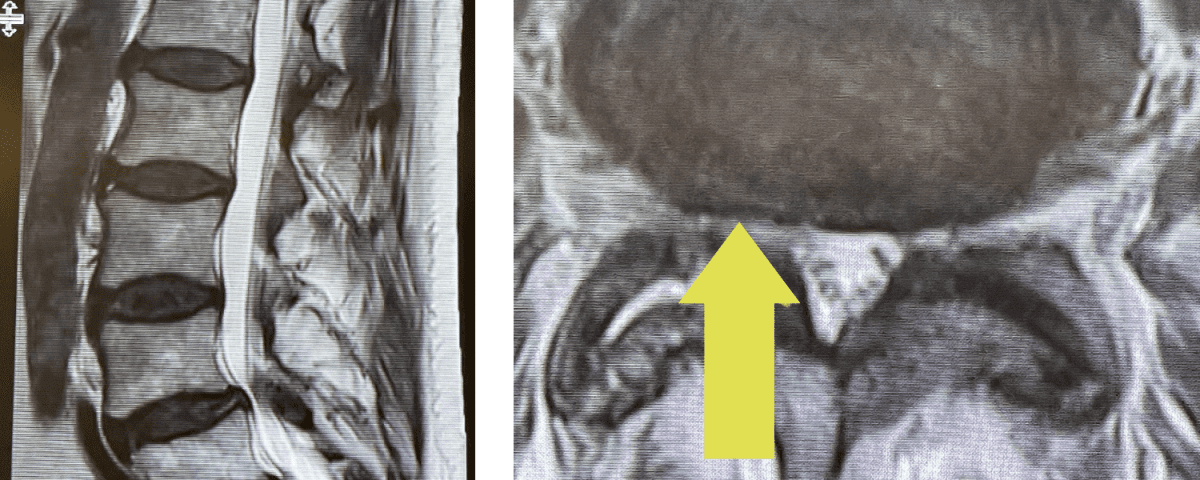
Figure 1 wjs 5 4
Yesterday I did a terrific case with my trusty orthopedic spine surgeon, Dr. Richard Obedian, with whom I have been working with as a team for the last twenty-one years. We are so close and work so well with each other. He anticipates every one of my moves and vice versa. We don’t even have to speak to each other to know what the other person wants. But we do speak, and we do communicate and have fun working with each other. This situation is what a patient wants and should have during their operation, and I believe this type of relationship offers the best care for the patient. Our practice prides itself on our relationships with the orthopedic surgeons. It is my wish for all of my spine neurosurgery colleagues to be working with an orthopedic spine surgeon. The patient gets the best of both worlds. Patients sometimes ask if they should see a neurosurgeon or an orthopedic surgeon. I will say that I am a bit biased. Our training is a bit different. Neurosurgeons have spine introduced to them on day one of their residency and make up the majority of cases they do during their experience. Orthopedic surgeons do have some spine surgery exposure but it is not usually the main thrust of their training and have traditionally been more involved in the fusion, instrumentation, and deformity correction such as scoliosis and not as much performing laminectomies or working with the nerves or spinal cord. They have to do a fellowship or extra training after residency to really practice spine surgery. Neurosurgery residencies these days have an infolded “spine fellowship” which gives the resident a great deal of exposure to deformity and instrumentation in addition to laminectomies and the more bread and butter stuff; there is not as much of a need to add on a spine fellowship although a lot do if they are interested in focusing on spine. Nevertheless people need to think of neurosurgeons when it comes to spine as much as our orthopedic colleagues.
I will tell you about the case study but first I want to clear up some important issues: Most people when they are told that they may need spine surgery are scared. And why shouldn’t they be? They have, for instance, a friend who had spine surgery and are never the same. Most people tell them they won’t walk or be paralyzed after surgery, applying this misconception whether it be cervical or lumbar. If the great majority of people did not do well after spine surgery word would get out and nobody would go for it. Neurosurgeons perform cervical surgery where, yes, the spinal cord is present at that level with an infinitesimally small risk of complication as per the literature and our own experience. Another point of misunderstanding in lumbar surgery is people don’t realize that there is no spinal cord below L1. Since most commonly spine surgery is performed at L2 and below you are at those levels only dealing with a sac of nerves floating in spinal fluid surrounded by a membrane and no spinal cord is present. One of the reasons I work as a team with an experienced orthopedic spine surgeon is a check and balance during our surgeries to ensure the safest and best technical care. We also have our own neuromonitoring company that monitors the nerve impulses from the patients toes to the brain to ensure what we are doing is safe. The important thing is to correlate the MRI findings to the patients symptoms and clinical exam.
CASE STUDY
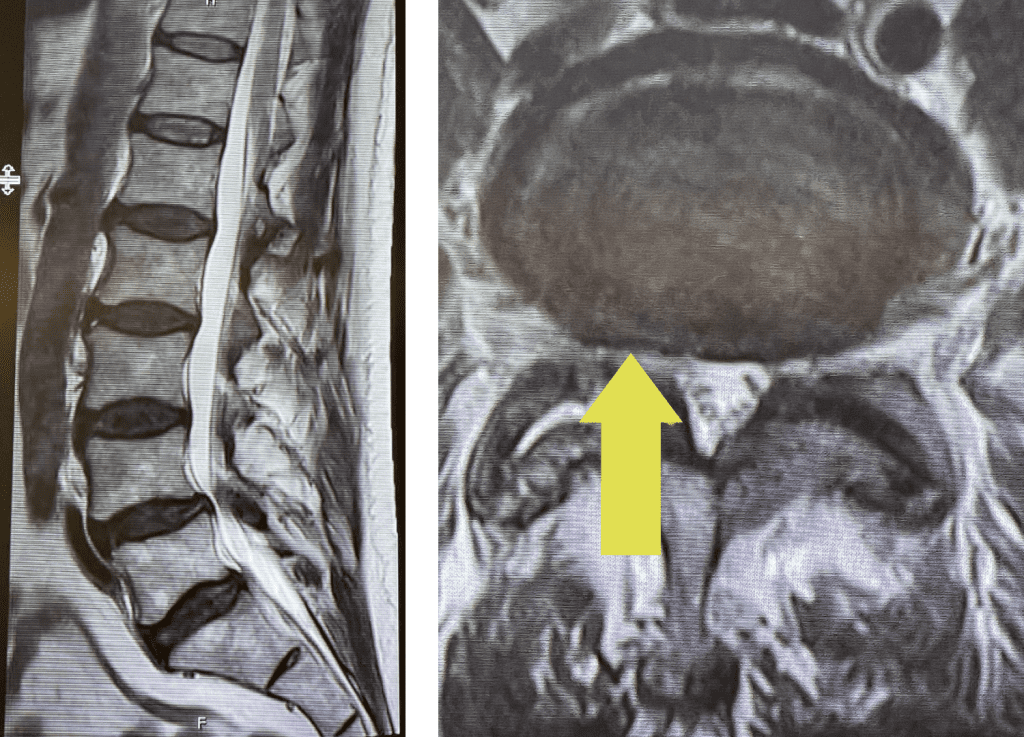
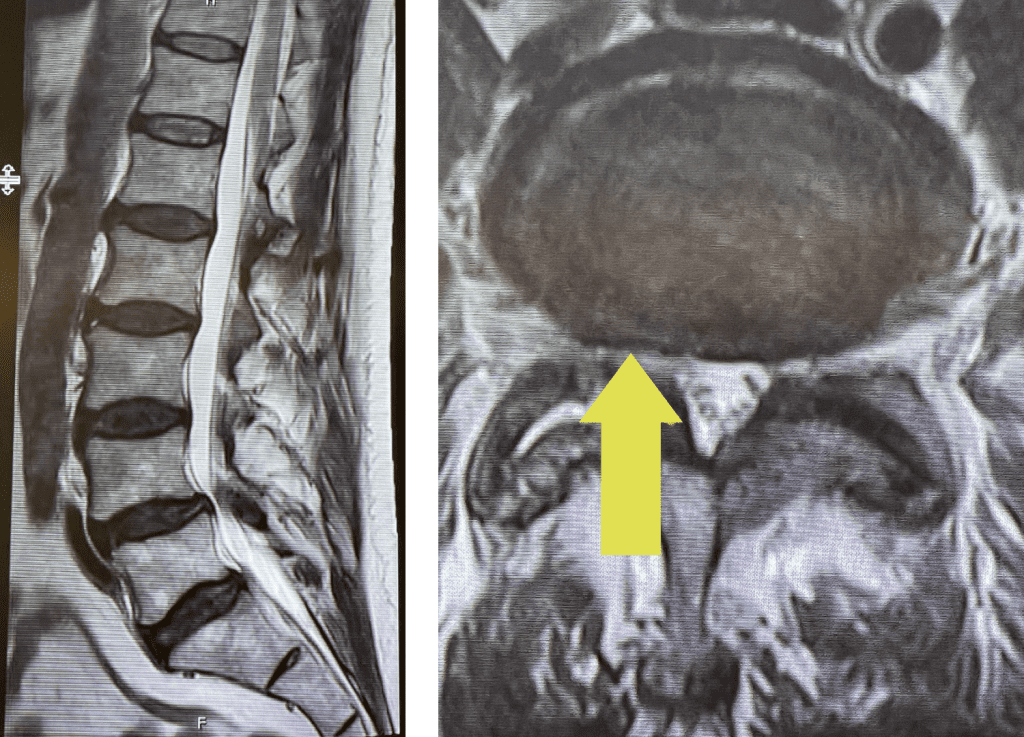
Fig 1: Sagittal and axial T2-weighted lumbar MRI demonstrating severe L4-5 Stenosis and grade 1 spondylolisthesis. Note (yellow arrow) cystic anteromedial extension off the right facet joint causing right-sided lateral recess cut-off of thecal sac and compression of the right L5 nerve root.
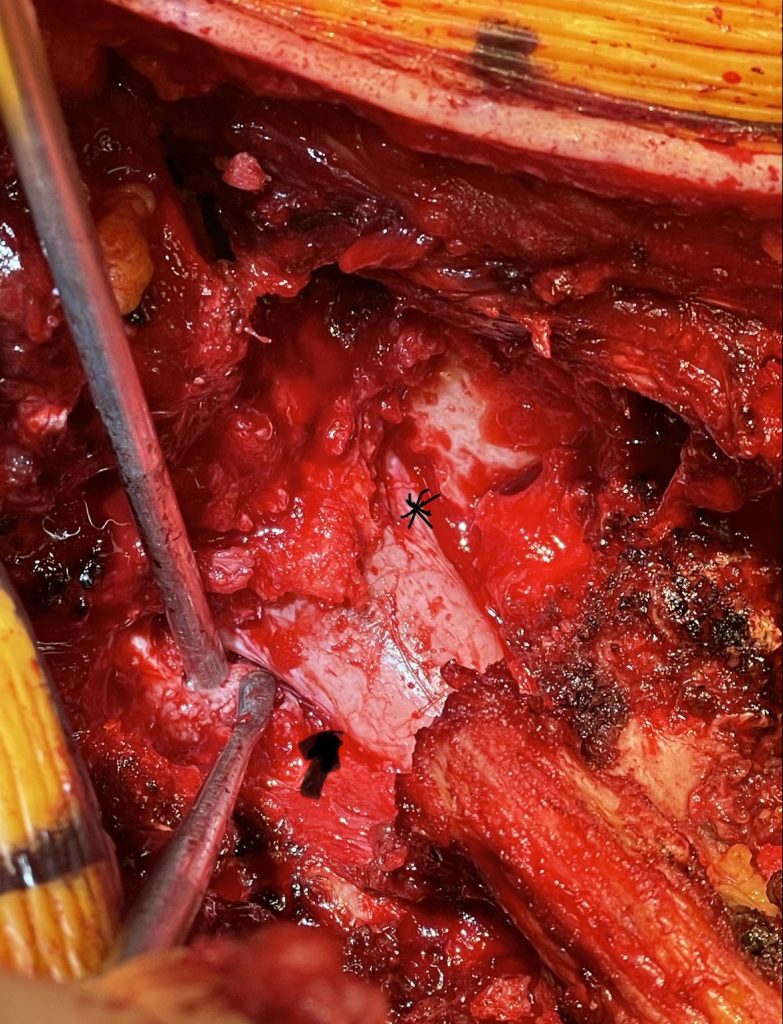
Fig 2: Intraoperative photo showing the thecal sac (arrow)completely decompressed after L3-5 laminectomy. Note the L5 nerve root very well decompressed (asterix)
This 70 year-old male with two years of right leg pain with minimal low back pain. The patient had tried physical therapy and epidural injections. Neurologically he was intact. MRI revealed a grade 1 spondylolisthesis (slipped spine in Greek) at L4-5 with severe lumbar stenosis mainly due to thickened yellow ligament and overgrown joints; but the thing that I believe put him over the edge was a small joint cyst on the right (Fig 1). People just form cysts. You can get a cyst in practically every organ including kidney, liver, ovarian, etc. People are actually fascinated by them. When patients have spine surgery the only thing that matters to them is, “did you get the cyst?” The fact is that they are these small gelatinous balls that come off the joint space and grow into the spinal canal and cause symptoms by compressing the nerve. You essentially bite them away with our instruments. You really can’t aspirate them through the skin. They are just a form of arthritis and are always benign.
During the surgery we perform what is called a decompressive laminectomy. Because he had the slip at L4-5 he required a fusion in addition. We elected to use screws with bone graft. People wonder what an actual laminectomy is. A laminectomy is a procedure to remove or “ectomy” the back ring of bone of the spinal segment .You literally bite it away with our special instruments. This bone is called the lamina. You do not need the lamina to live, like an appendix. There are gaps between each lamina segment going up the spine to begin with and there is a tremendous amount of tissue including muscle so one is protected, and it is ok to do this. You need to do the laminectomy to shave away the material that is both hard and soft that is compressing the sac of nerves. Your goal in the surgery is to make the sac nice and round again with a normal diameter. Since in the lumbar spine there is no spinal cord you are dealing with the peripheral nervous system not the central nervous system like the brain and spinal cord. A sac of nerves floating in fluid is a protected system, like a baby in amniotic fluid. At the same time you must not only remove the pressure on the sac, but also you must shave away the pressure on the nerve roots as well, which is called a foraminotomy (Fig 2). The nice thing about a fusion is you can be aggressive in the amount of decompression and joint removal you can do because you are fixing chronic as well as iatrogenic acute instability.
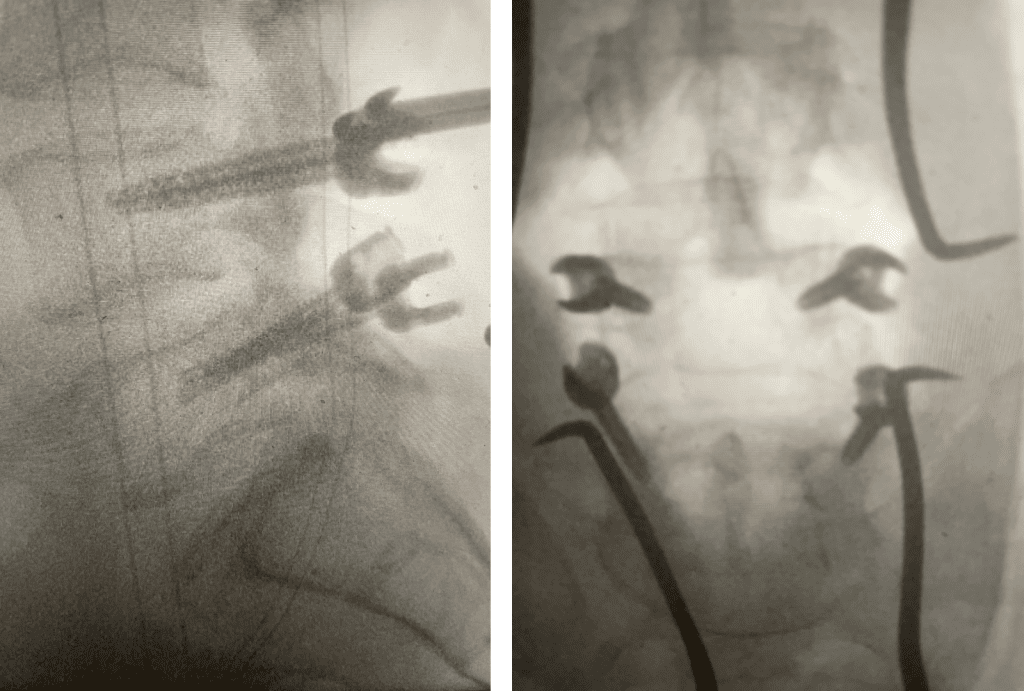
Fig 3: Intraoperative lumbar fluoroscopic lateral and AP images demonstrating good screw placement in performing an L4-5 fusion.
During the surgery we encountered the “cyst” as it was coming from inside or medial joint space between the two bony processes that make up the facet joint itself, like two puzzle pieces that fit together with a synovial-lined space that can for a degenerative synovial cyst. The cyst is like a pimple and actually is quite satisfying to pop and release the material that looks like curd as it is rarely liquid. Because of the consistency and the location, they are not really able to be aspirated or found. After we did what we set out to do which was to make the nerve sac without any pressure as well as the L5 nerve roots, which are most affected at this level. We performed a fusion with two titanium screws in L4 and two in L5, which were connected by rods that were bent or lordosed (Fig 3). They are easy to put in and serve the purpose of connecting the two levels to prevent any relative motion or translation of L4 on L5. This also most importantly prevents the body from signaling the spine to make arthritis to attempt to auto stabilize itself. After the surgery the patient had relief of his right leg pain and had an uneventful postoperative course.
Patients often worry about their mobility after spine surgery. What they don’t realize is how amazing the body is able to compensate even for a multilevel fusion. In my experience for a one or two level fusion, people do not experience an appreciable difference in mobility if their back pain and dysfunction is relieved. They may in fact experience an improvement in their mobility if their low back pain is improved. In the first place their spinal segment was not working properly to begin with; it was only causing the patient harm. It has also been my experience that if a patient’s horrible leg pain is relieved or significantly improved they are quite happy. This type of pain is much more intolerable to most patients; patients seem to have the ability to tolerate the low back symptoms more than this terrible leg pain and particularly with progressive weakness.