- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Brain Metastasis
A woman with rapid deterioration in vision – Meningioma
October 26, 2021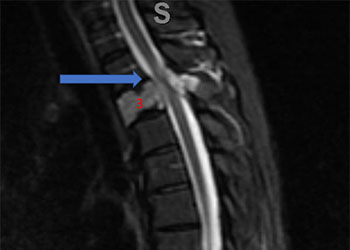
Spinal Embolization Treats Aggressive Comprehensive T3 Verterbral Body Hemangioma
October 26, 2021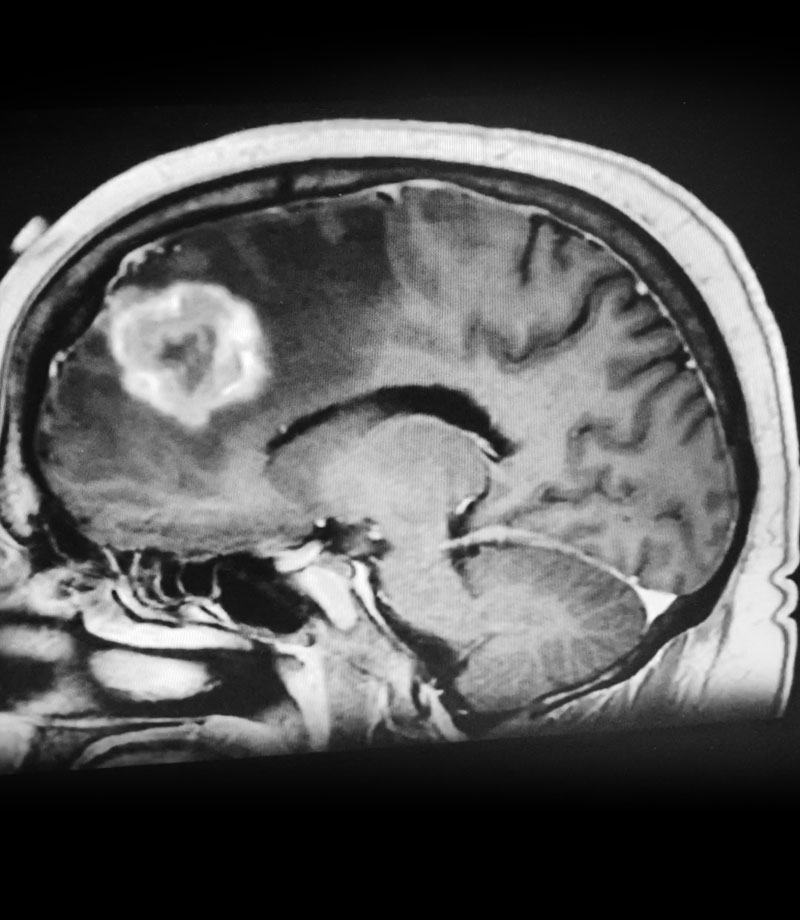
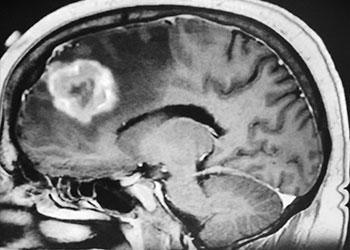
Figure 1: Sagittal post-contrast MRI.
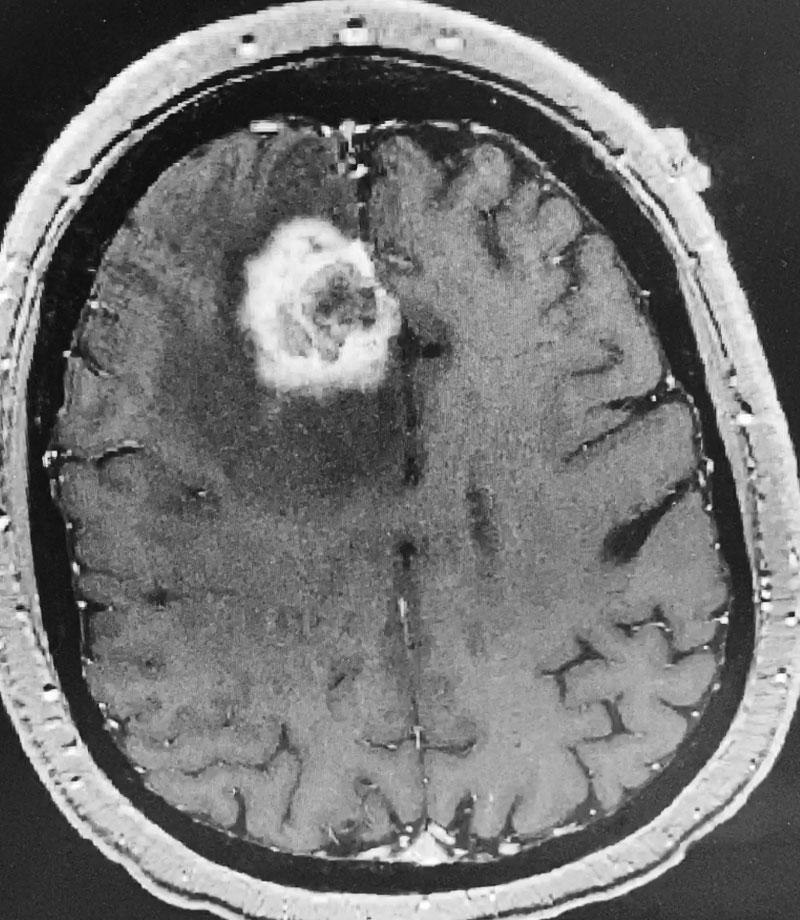
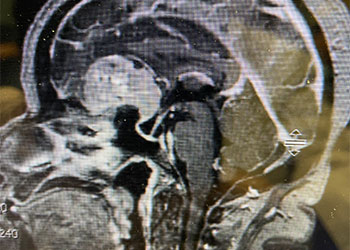
Figure 2: Axial post-contrast MRI.
Postoperative images looked good (Figure 3). The patient felt better after surgery. His headaches were much better and he started to feel stronger. He was discharged after a brief hospital stay. He tapered his steroids to off. He will get follow up MRI images every few months. If tumor does recur, repeat radiosurgery would be performed.
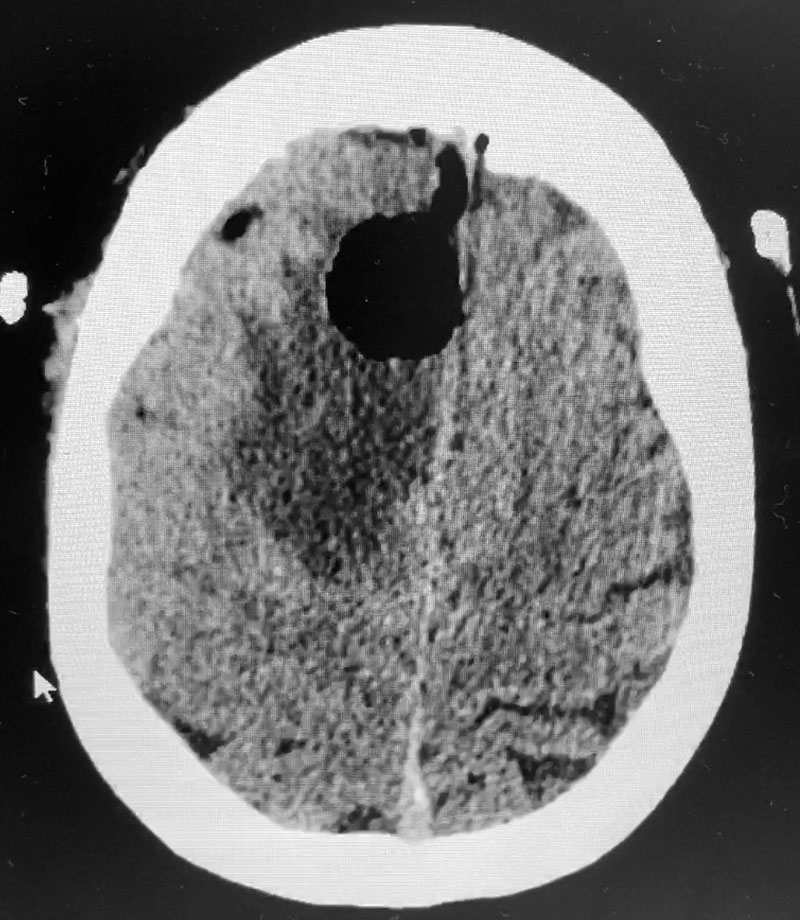
Figure 3: Post operative CT scan.
Brain metastases are common in patients with cancer. As cancer therapies improve, we are seeing more metastatic brain disease. The systemic disease is often better controlled with chemotherapy, but the chemotherapy generally doesn’t get into the brain because of the “blood-brain barrier,” a special protection the brain has against exposure to various chemicals in the blood. Therefore, brain disease can develop and progress despite successful control of disease everywhere else.
Most brain metastases are effectively treated with Gamma Knife, a one day stereotactic radiosurgery treatment. Gamma Knife is effective for all types of metastatic disease including tumors that are traditionally considered “radioresistant” like melanoma, renal cell carcinoma, and sarcoma. Gamma Knife can also treat up to about 10 metastatic tumors in one sitting. Gamma Knife can also be repeated over time if tumors recur or if new tumors develop.
Patients with more than 10 brain metastases are usually treated with “whole brain radiation therapy” (WBRT) over several weeks. Patients with a single, large, accessible brain metastasis may do best with surgical removal of the tumor.
Months or years after stereotactic radiosurgery treatment, a phenomenon called “radiation necrosis” can occur. In this case, an enhancing mass can be seen at the site of radiation treatment with surrounding edema and symptoms that can all mimic recurrent tumor. Radiation necrosis can usually be treated with steroids and hyperbaric oxygen, though in rare cases, surgery may be necessary.
This patient seemed to be an appropriate surgical candidate given that he was otherwise healthy, had controlled systemic disease, had already had 2 treatments of radiosurgery, and was highly symptomatic with a large superficial mass. Also, it was unclear whether the mass was recurrent tumor or radiation necrosis, though usually a combination is present. The final pathological diagnosis in this case was metastatic cancer, consistent with lung primary, with extensive necrosis.
CATEGORY: BRAIN // BRAIN METASTASIS
Brain Metastasis
This is a 59 year-old man who had been diagnosed with Non-small cell lung cancer. In the past year and a half, he had undergone stereotactic radiosurgery twice for what appeared to be a right frontal brain metastasis. Three months earlier, there was an increase in the size of the mass with increased surrounding edema. The possibility of radiation necrosis was raised, and the patient underwent a course of hyperbaric oxygen treatment as well as oral decadron (dexamethasone).
The patient subsequently had increased headaches and weakness. MRI showed the mass had increased further, with persistent surrounding edema (Figure 1). Systemic work-up showed no active metastatic disease. It was suspected that there was recurrence of metastatic tumor as well as some component of necrosis (Figure 2). The patient underwent a right frontal craniotomy, by Dr. Michael Brisman, with brainlab stereotactic guidance. A cortical incision was made right over the mass. The mass was consistent primarily with metastatic tumor. The tumor was surgically removed.