- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Cervical Laminectomy and Fusion
Grade II Oligodendroglioma
October 27, 2021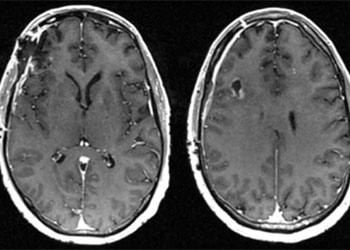
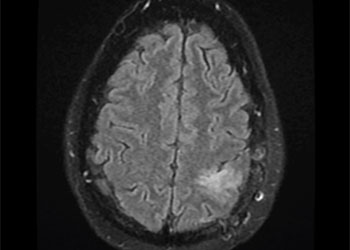
Cerebral Metastases from Non-Small Cell Lung Cancer
October 27, 2021An MRI (Fig. 1) demonstrated severe stenosis at C2-3 with cord compression secondary to significant thickened posterior ligament and facet arthropathy. The patient had a posterior cervical laminectomy C1-3 to decompress the spinal cord and instrumented fusion C2-4.On exploration, the patient was deemed to be fused and the previous hardware was removed except for the lateral mass screws at C3 and C4 were left in. Postoperatively the patient had an uneventful course with some improvement in finger extensor strength.
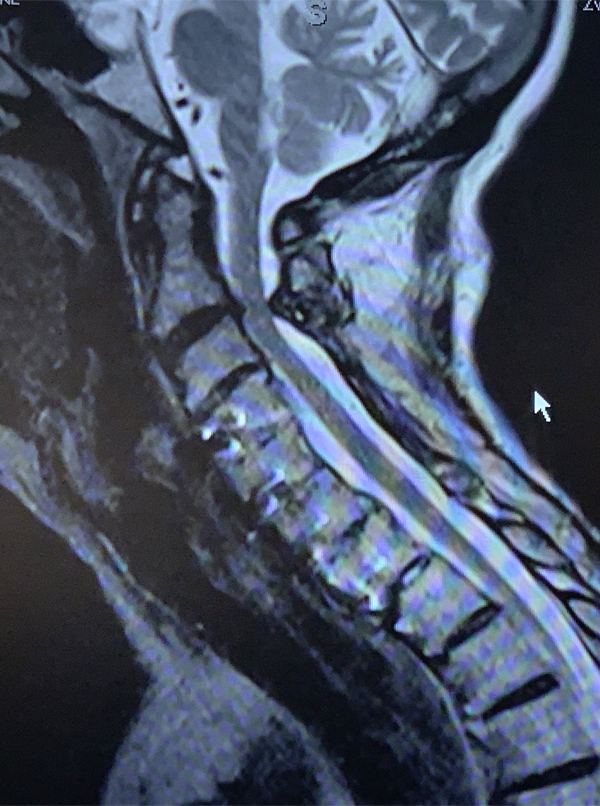
Figure 1: Sagittal T2 MRI of the cervical spine demonstrates severe spinal cord compression at C2-3 above prior to instrumented decompression and fusion.
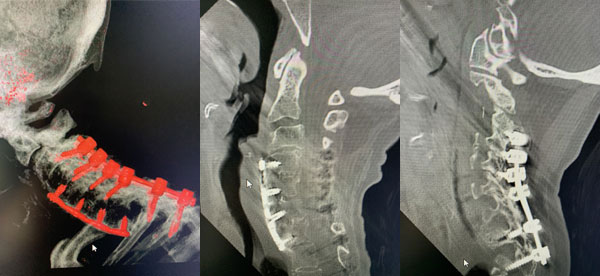
Figures 2a, b, c: Preoperative sagittal CT scans of the cervical spine demonstrating preoperative instrumentation. Note degenerative changes and anteriolisthesis of C2 and C3.
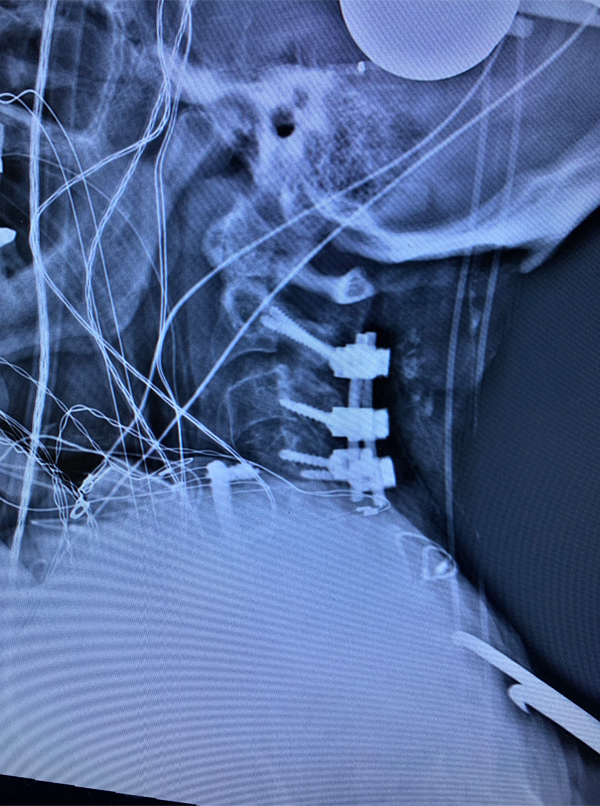
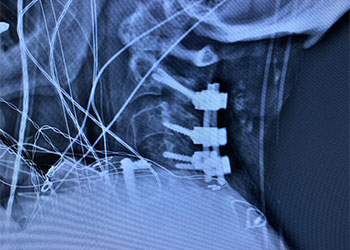
Figure 3: Postoperative lateral c-spine x-ray showing removal of prior long posterior construct with final short segment fusion C2-C4. Note addition of bilateral C2 pars screws.
KEY LEARNING POINTS:
- Patients with cervical spondylotic myelopathy develop spinal cord compression secondary to arthritic changes of the structures surrounding the spinal canal. Arthritis is a compensatory mechanism of the body to chronic instability.
- This is due to abnormal biomechanics of the spinal motion segment. due to degenerative loss of cartilaginous or ligamentous laxity. The result is thickened and/or hypertrophied structures that compromise the spinal canal as was in this case or nerve foramina.
- Patients may have chronic subluxation both antero or retrolisthesis of the spinal segment.
- Upper spinal cord compression can present with a myriad of symptoms: A) They can present with or without neck pain. B) They can develop numbness of their hands or fingers. They can describe a gravely or sandpaper-like sensation and often will have difficulty buttoning their shirt or lose their sense of position of their hands in space. This is often coined “myelopathy hand.”
- Approximately 5-10 percent of patients with cervical spondylotic stenosis will develop frank myelopathy which can develop slowly or patients may rapidly deteriorate.
- Long tract weakness may develop which often consists of weakness of triceps or finger extensors or lower extremity proximal hip flexor or dorsiflexor weakness. They may have gait abnormalities.
- Patients may be hyperreflexia and/or have a Hoffman’s or Babinski sign. These UPPER MOTOR NEURON signs are secondary to the release of more primitive spinal cord tracts as a result of inhibition of the corticospinal tracts.
- MRI or CT myelogram findings may consist of either anterior or posterior compression or both from a variety of degenerative pathologies including severe ligamentous hypertrophy, calcification or ossification of the posterior longitudinal ligament, disc osteophyte complex, facet hypertrophy, or next segment degeneration and/or luxation secondary to a prior fusion procedure.
- Areas of the spinal cord with compression may have evidence of myelomalacia which is often revealed as a hyperintensity on T2- weighted images and represent an area of chronic spinal cord damage on MRI.
- The age range for patients to develop these chronic changes are in the 50-70 year range; however, there are younger patients who have a congenitally narrow spinal canal, to begin with, and more readily develop spondylotic changes that result in spinal cord compression. Patients with early signs of myelopathy can be followed closely to see if any changes occur.
- Patients can try physical therapy to improve their strength and/or pain management if neck pain is a major component of their symptoms. Patients with the progression of symptoms or signs or present with significant long tract weakness and/or abnormal reflexes should undergo surgical decompression of the spinal cord.
- This may be accomplished through either an anterior or posterior approach depending on the pathology and whether the patient has a kyphotic or lordotic position of the cervical spine.
- Patients with significant anterior compression and multiple levels involved, but have a good lordosis, may successfully be decompressed through a posterior approach or laminectomy. Often a fusion procedure with instrumentation is done in order to provide stability and good long-term alignment.
- The most important reason for surgical decompression is to prevent a patient from getting worse and preserve neurological function. Depending on the length of symptoms, neurological exam, age, and degree of spinal cord compression and myelomalacia will dictate the extent of neurological recovery. As a rule, patients improve from decompression. Overall patients have about a 70- 75% improvement of symptoms and signs.
CATEGORY: SPINE // CERVICAL LAMINECTOMY AND FUSION
Cervical Laminectomy and Fusion
The patient is a 66-year-old female who presents with 2 months of progressive difficulty ambulating and using her hands. She was noted to have long track weakness.
She had a prior history of having a C4-C7 anterior cervical discectomy and fusion. She subsequently developed a listhesis of C7-T1 necessitating a posterior laminectomy and fusion from C3-T2.