- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Minimally Invasive Approach for Spinal Revision Surgery
Sudden Coma While Receiving Physical Therapy
October 26, 2021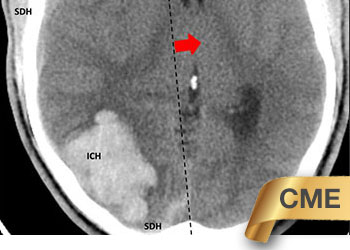
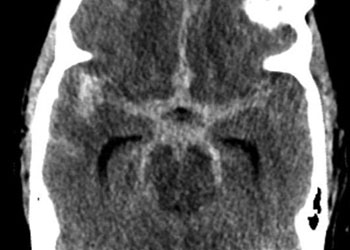
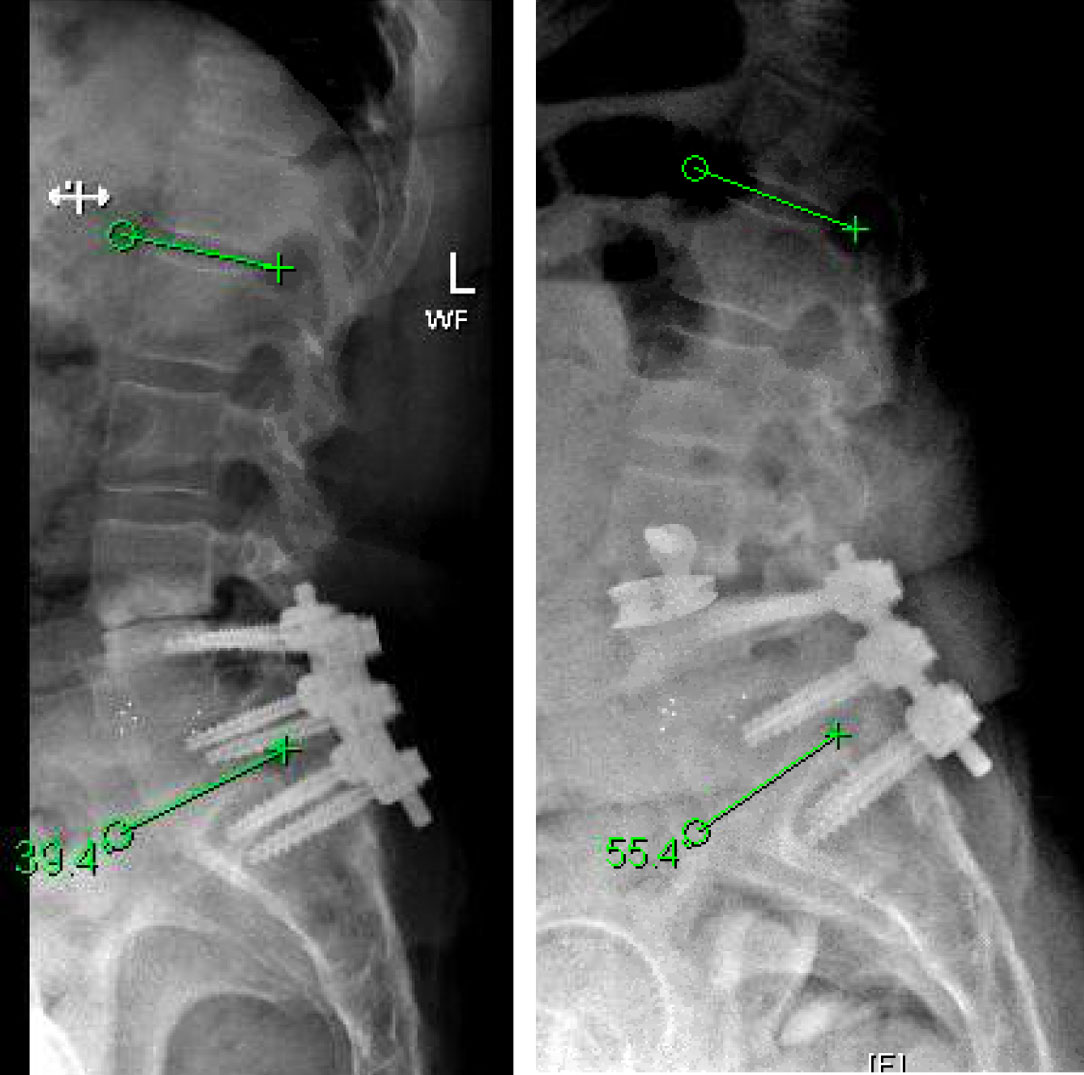
Young college student with severe headache and a large intracerebral bleed
October 27, 2021The goals of surgery were to achieve spinal stability, neural decompression, and re-establish a physiologic sagittal alignment. She had co-morbidities that precluded a more conventional open posterior approach with hardware revision. We therefore elected to perform an L3-4 Minimally Invasive Direct Lateral Interbody Fusion with Plate. This allowed for stability through the interbody device and lateral plate, indirect neural decompression by distracting the spinal canal and neuroforamina, and increase lordosis by lengthening the anterior aspect of the spine with placement of a hyperlordotic cage.
Patient tolerated the surgery well and attained near complete relief of her preoperative leg pain and chronic back pain. Incision was a little over one inch on her lateral side. Her postoperative pain was less significant given the indirect access to the spine which allowed for preservation of her paraspinal musculatures, and minimally invasive approach which maintained the integrity of the lateral muscle. She was discharged home on the day after surgery and was able to fully wean off her chronic narcotics.
Xavier P. J. Gaudin
References:
Levin DA, Hale JJ, Bendo JA. Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis. 2007;65(1):29–36. https://pubmed.ncbi.nlm.nih.gov/17539759/
Louie PK, Varthi AG, Narain AS, Lei V, Bohl DD, Shifflett GD, Phillips FM. Stand-alone lateral lumbar interbody fusion for the treatment of symptomatic adjacent segment degeneration following previous lumbar fusion. Spine J. 2018 Nov;18(11):2025-2032. https://pubmed.ncbi.nlm.nih.gov/29679730/
Malham GM, Ellis NJ, Parker RM, Blecher CM, White R, Goss B, Seex KA. Maintenance of Segmental Lordosis and Disk Height in Stand-alone and Instrumented Extreme Lateral Interbody Fusion (XLIF). Clin Spine Surg. 2017 Mar;30(2):E90-E98. https://pubmed.ncbi.nlm.nih.gov/28207620/
Ohba T, Ebata S, Haro H. Comparison of serum markers for muscle damage, surgical blood loss, postoperative recovery, and surgical site pain after extreme lateral interbody fusion with percutaneous pedicle screws or traditional open posterior lumbar interbody fusion. BMC Musculoskelet Disord. 2017 Oct 16;18(1):415. https://pubmed.ncbi.nlm.nih.gov/29037186/
CATEGORY: SPINE // MINIMALLY INVASIVE APPROACH FOR SPINAL REVISION SURGERY
Minimally Invasive Approach for Spinal Revision Surgery
This is a 55 year-old-female who presented with progressively worsening axial low back pain and left lower extremity radiculopathy. She had a previous L4 to S1 posterior laminectomy with interbody fusion by another spine surgeon about three years prior. Imaging demonstrated L3-4 adjacent segment degeneration with spinal instability and stenosis. She additionally developed subsidence from her initial surgery, which resulted in loss of physiologic lordosis and presumptively accelerated the adjacent degenerative process. Her L4-S1 construct otherwise appeared to have a solid arthrodesis. Symptoms were debilitating and she had failed best medical management, therefore surgery was offered.
Authors
To learn more about the author, click his name or photo:

