- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Octogenarian with mild dizziness and headache
Symptomatic Near-Occlusion of the Carotid Artery
October 27, 2021
Spinal Embolization Treats Aggressive Compressive T3 Vertebral Body Hemangioma
October 27, 2021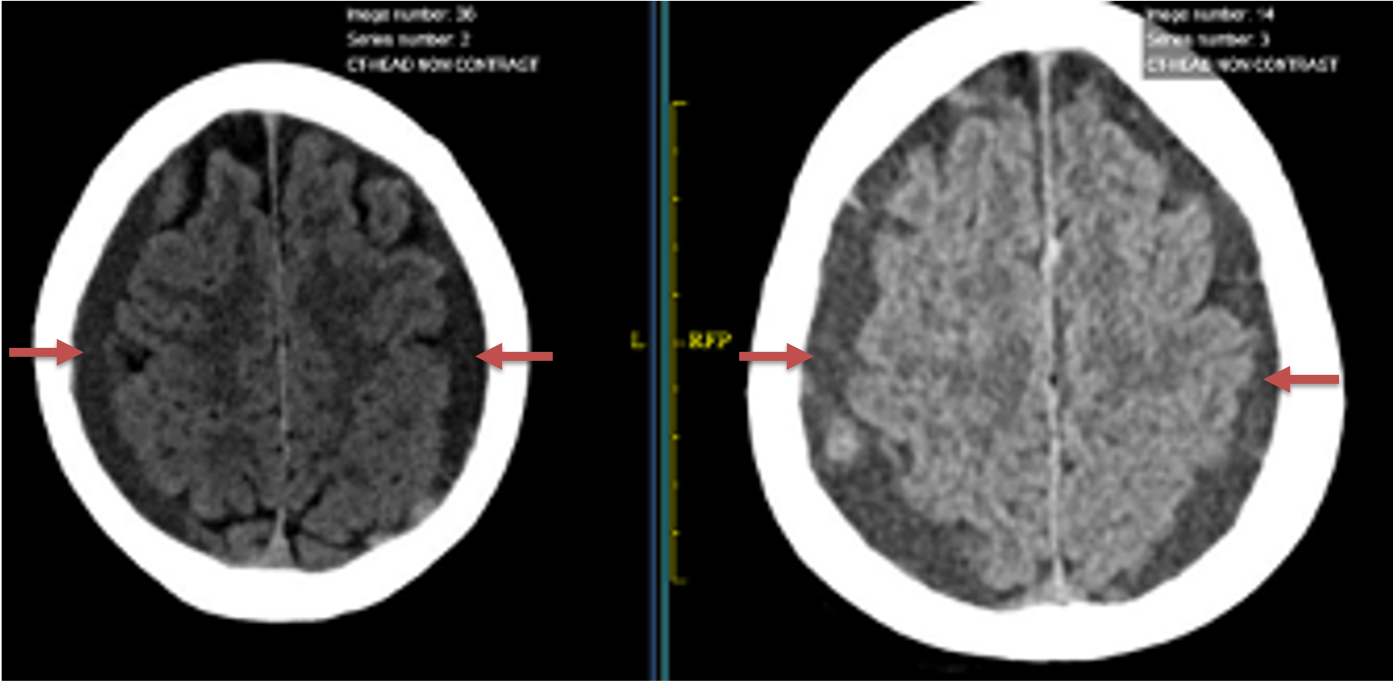
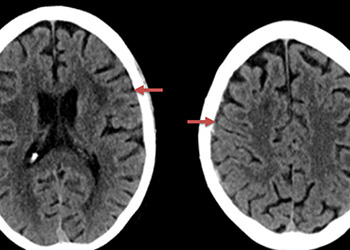
Figure 1. A) 6 weeks post mild trauma B) 4 weeks post mild trauma demonstrate stable subacute subdural collections with mild growth and sulcal effacement.
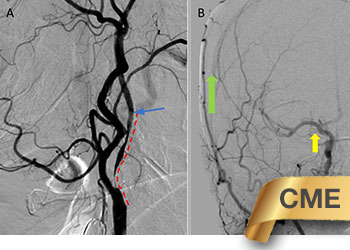
The patient agreed to receive minimally invasive treatment with Bilateral Middle Meningeal Artery Embolization, a new approach to promote resorption of chronic and subacute subdural hematomas in patients that are not improving with conservative measures or have contra-indications to surgical evacuation. Selective catheterization of the Middle Meningeal Artery is followed by transarterial embolization of the territory and inflammatory membranes that are felt to be secreting serosanguinous proteinaceous exceeding the capacity for resorption. MMA embolization was performed bilaterally in this patient. (Figure 2. A and B)
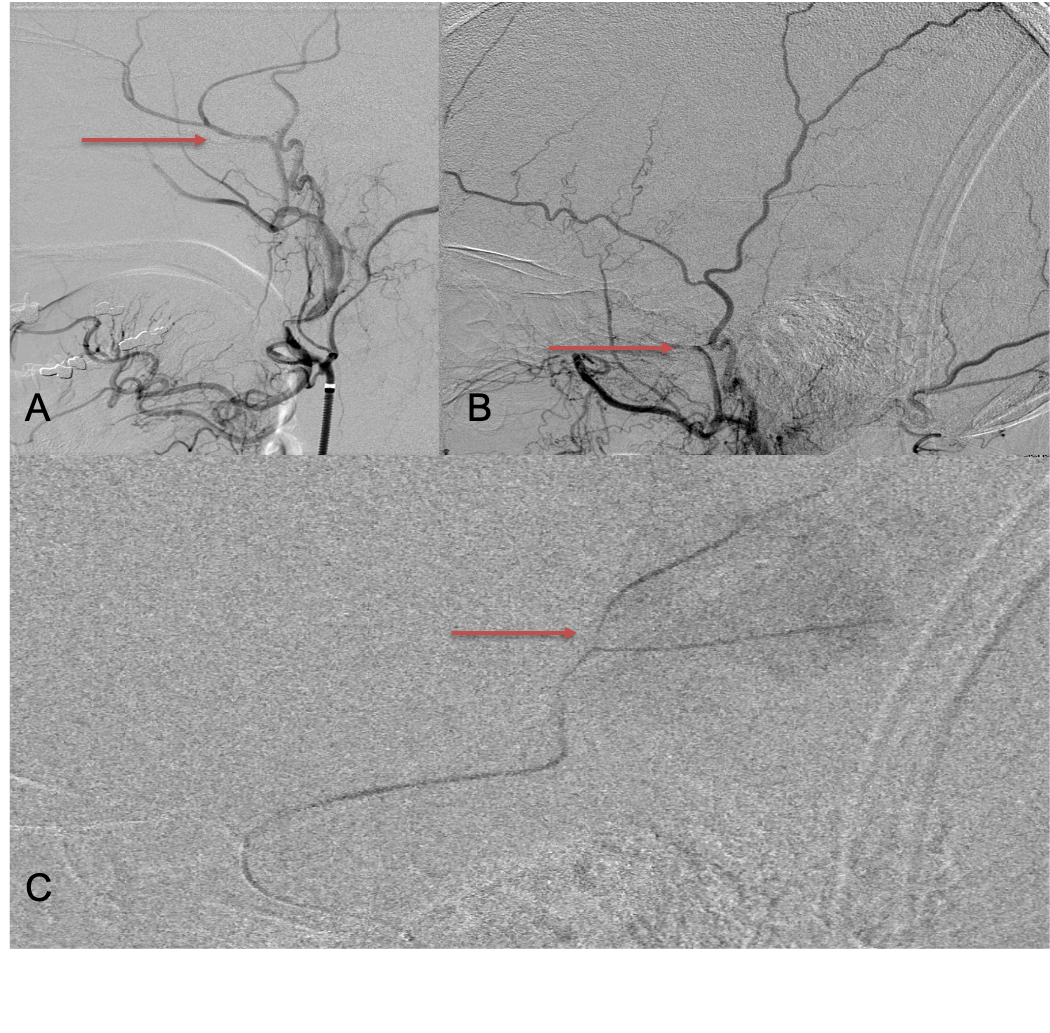
Figure 2. A) Initial right ECA angiogram ; B) Post MMA Embolization; C) Selective Embolization Of Middle Meningeal Artery Membranes using PVA particles (arrows)
CT follow-up at 1 week demonstrates early resorption. 2 weeks post MMA embolization, resolution of the left subdural collection with new small thin acute hemorrhage in an otherwise stable right subdural collection is observed (Figure 3. A and B).
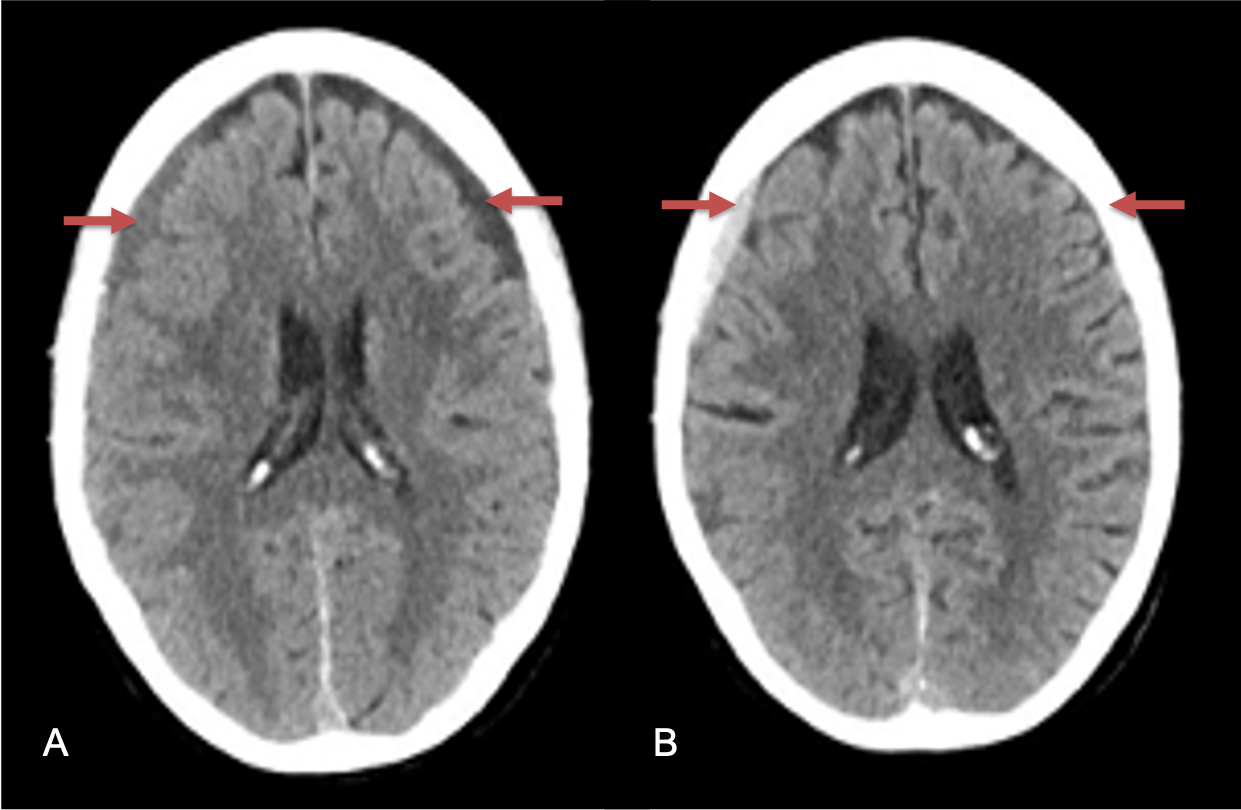
Figure 3. A) 1 week post MMA embolization demonstrating decreasing thickness bilaterally B) 2 weeks post MMA demonstrates resolution on left, with small new acute component on right with overall decreased thickness.
Clinically, the patient improved over the few weeks with the occasional transient twinge of a headache, but resolution of dizziness. Follow-up CT at 10 weeks demonstrated complete resolution of the bilateral subdural hematomas with our patient complete symptomatic and back to all of his activities of daily living. Considering his history of thrombocytopenia and CLL, we will continue to monitor him into the future and are excited about his progress and recovery. (Figure 4. A and B)
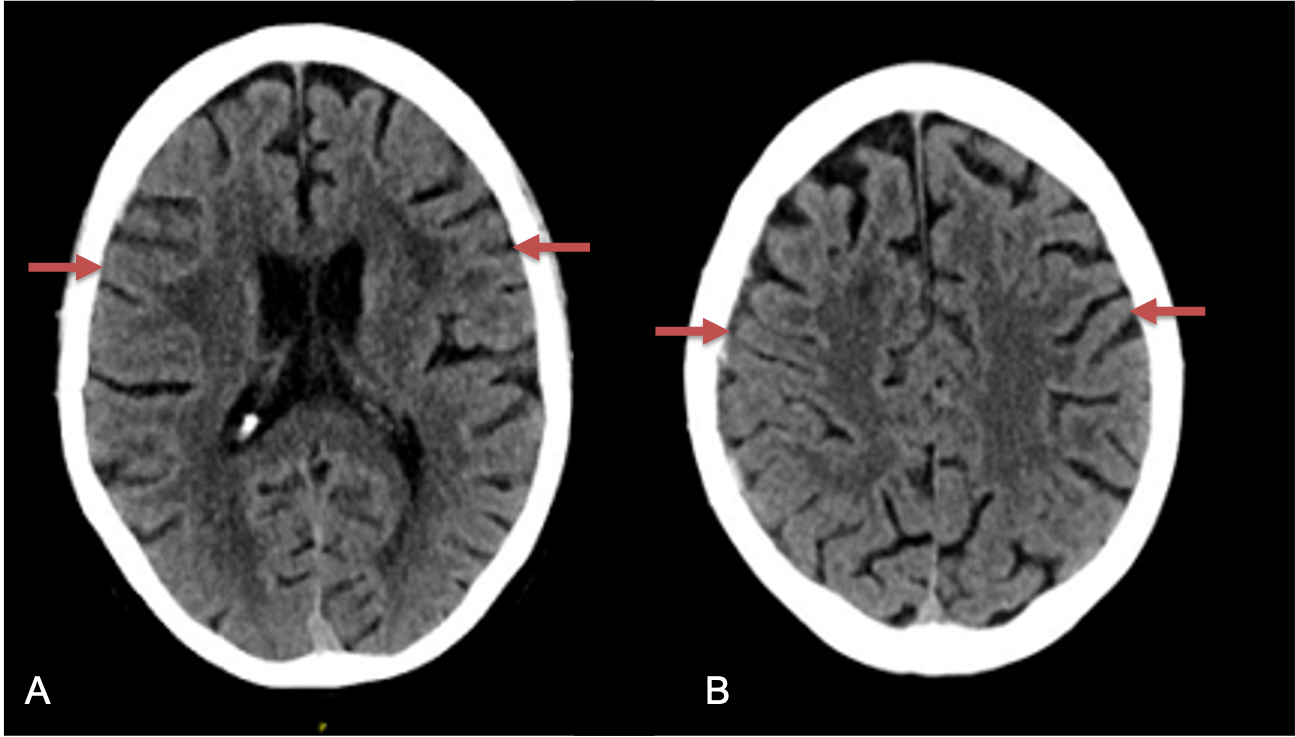
Figure 4. A and B) – 10 weeks following embolization demonstrates complete resolution of bilateral collections both acute and chronic.
Discussion:
Chronic and subacute subdural hematoma is a very common neurosurgical condition. Although conventional surgical methods, such as burr hole irrigation or observation in asymptomatic patients have been the mainstay of treatment, middle meningeal artery (MMA) embolization has emerged as a promising adjunctive or alternative treatment. Several double arm and single arm studies comparing embolization and conventional surgery groups have been published (References 1 and 2). In the meta-analysis performed by Srivatsan etal., hematoma recurrence rate was significantly lower in the embolization group compared with conventional treatment group (2.1% vs. 27.7%; odds ratio = 0.087; P < 0.001) in carefully selected minimally or asymptomatic patients; surgical complication rates were similar between groups (2.1% vs. 4.4%). The composite hematoma recurrence rate of 3.6% was found after summing the case series in their analysis, which were lower than published values of conventional observation and surgical treatments in this carefully selected group of chronic and subacute minimally symptomatic patients.
References:
- Ban SP, Hwang G, Byoun HS, Kim T, Lee SU, Bang JS, Han JH, Kim CY, Kwon OK, Oh CW. Middle Meningeal Artery Embolization for Chronic Subdural Hematoma. Radiology. 2018 Mar;286(3):992-999. doi: 10.1148/radiol.2017170053. Epub 2017 Oct 10. PMID: 29019449.
- Srivatsan A, Mohanty A, Nascimento FA, Hafeez MU, Srinivasan VM, Thomas A, Chen SR, Johnson JN, Kan P. Middle Meningeal Artery Embolization for Chronic Subdural Hematoma: Meta-Analysis and Systematic Review. World Neurosurg. 2019 Feb;122:613-619. doi: 10.1016/j.wneu.2018.11.167. Epub 2018 Nov 24. PMID: 30481628.
CATEGORY: ENDOVASCULAR // MIDDLE MENINGEAL ARTERY EMBOLIZATION OF LARGE SUBACUTE SUBDURAL HEMATOMAS
Octogenarian with mild dizziness and headache
Case Presentation:
A man in his 80s developed mild dizziness and headache following incidental trauma working in his garage one day. He presented several weeks later to the ER and was diagnosed with bilateral subdural hematomas, which were initially managed with observation, low dose Decadron, considering the mildness of symptoms, advanced age, and history of CLL with thrombocyptopenia (<100k). Over the next 4 weeks, the collections remained relatively stable with evidence of slight growth (10 to 12 mm thickness, and 2 mm right to left shift) on NCT (Figure 1. A and B).