- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Thoracic Spinal Cord Tumor Case Presentation
A woman with rapid deterioration in vision – Meningioma
October 26, 2021Surgery was offered for spinal cord preservation, neurologic preservation, symptomatic management, histopathologic diagnosis, and to decrease the tumor burden. Dr. Gaudin performed an uneventful T7-T9 motion-sparing laminectomy with complete resection of T8 intradural extramedullary tumor. The intraoperative neurophysiologic motor and sensory evoked potentials remained stable. Her postoperative course was unremarkable, and she was discharged home on postoperative day 3.
Pathology came back as Atypical Meningioma, WHO grade 2. Postoperative MRI showed a gross total resection without residual tumor, and appropriate spinal cord re-expansion. On her most recent follow-up at 6 weeks, she was very pleased with the results from the surgery. She reports resolution of her preoperative thoracic back and radicular pain, and great improvement with her ability to ambulate and overall function. It is demonstrated by her interval VAS of 2/10, and ODI of 23/100. She is expected to continue improving with time and therapy. Follow-up plan is to observe with radiographic surveillance.
While meningiomas are the most common primary intracranial tumors, spinal meningiomas are relatively rare and account for about 1.2% of all meningiomas. They have a predilection for the thoracic spine and female gender. They are most often benign and slow-growing, therefore usually reach a distinct size with significant spinal cord compression at time of diagnosis. Maximum safe resection is the preferred treatment when there is radiographic compression and neurologic compromise. The recurrence rate ranges from 10 to 13%. Adjuvant radiation can be an option for incomplete resection or recurrent tumors.
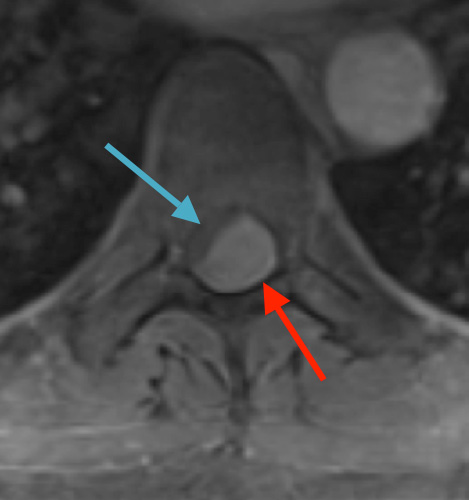
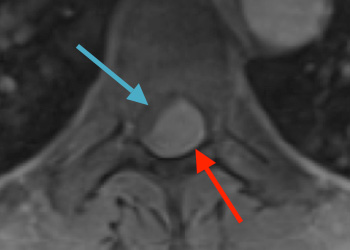
Preoperative MRI T1w demonstrating a large enhancing tumor (red arrow) causing severe cord compression and displacement (blue arrow)
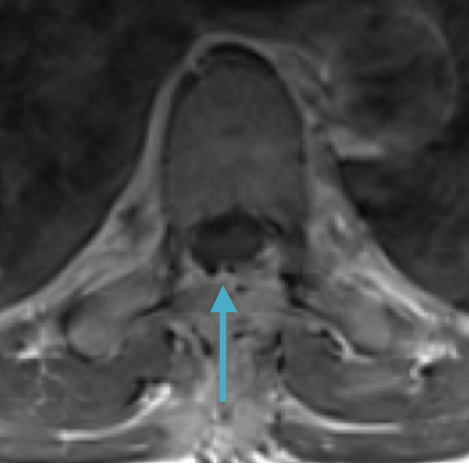
Postoperative MRI T1w demonstrating interval resection with cord re-expansion (blue arrow)

Preoperative MRI T2 demonstrating obstruction of CSF around the cord (blue arrow), resulting from the tumor (red arrow)

Postoperative MRI T2 illustrating the restoration of CSF surrounding the cord (blue arrow)

Preoperative MRI T1w demonstrating a large enhancing tumor with severe cord compression

Postoperative MRI T1w demonstrating a gross total resection
References:
Sandalcioglu IE, Hunold A, Müller O, Bassiouni H, Stolke D, Asgari S. Spinal meningiomas: critical review of 131 surgically treated patients. Eur Spine J. 2008;17(8):1035-1041.
https://pubmed.ncbi.nlm.nih.gov/18481118/
Gezen F, Kahraman S, Canakci Z, Bedük A. Review of 36 cases of spinal cord meningioma. Spine (Phila Pa 1976). 2000 Mar 15;25(6):727-31
https://pubmed.ncbi.nlm.nih.gov/10752106/
Riad H, Knafo S, Segnarbieux F, Lonjon N. Spinal meningiomas: surgical outcome and literature review. Neurochirurgie. 2013 Feb;59(1):30-4.
https://pubmed.ncbi.nlm.nih.gov/23395186/
CATEGORY: SPINE // THORACIC SPINAL CORD TUMOR
Thoracic Spinal Cord Tumor Case Presentation
This is a 55-year-old female with no past medical history who presented electively with a 10 month history of progressively worsening mid back pain radiating across the chest, and gait disturbance. Pain was especially worse at night and when laying flat. Her exam was pertinent for severe ataxia when ambulating, and elevated deep tendon reflexes in the lower extremities. She had severe and debilitating symptoms, as demonstrated by her Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) of 9/10 and 64/100, respectively. MRI of the thoracic spine with and without contrast demonstrated a large intradural extramedullary homogenously enhancing mass at T8, resulting in near obliteration of the spinal canal and severe cord compression. She was referred to Dr. Xavier Gaudin for neurosurgical management.
Authors
To learn more about the author, click his name or photo:

