- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Lateral Recess Stenosis
NSPC Neurosurgeon Dr. Jonathan Brisman Now On Staff At Lenox Hill
June 20, 2022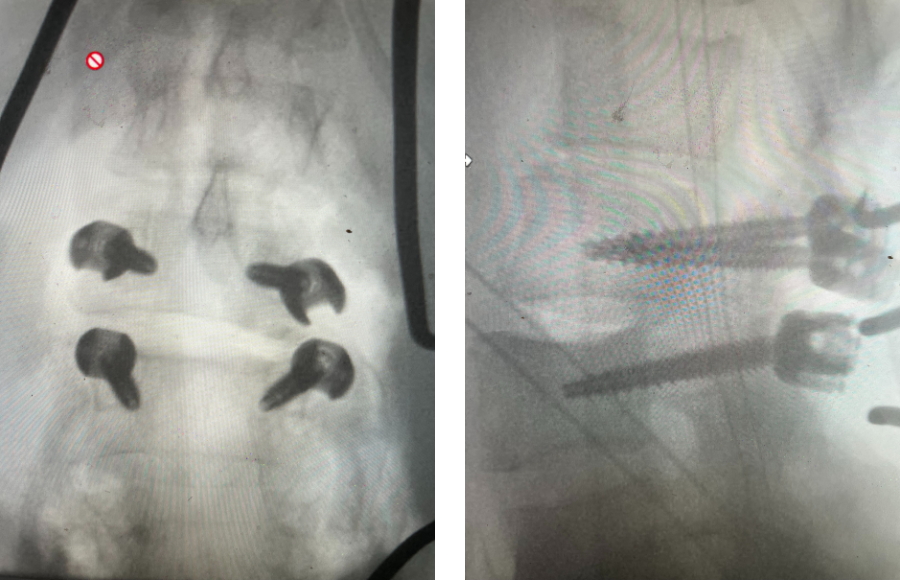
Sometimes It Is Obvious And Sometimes It Is Not
June 10, 2022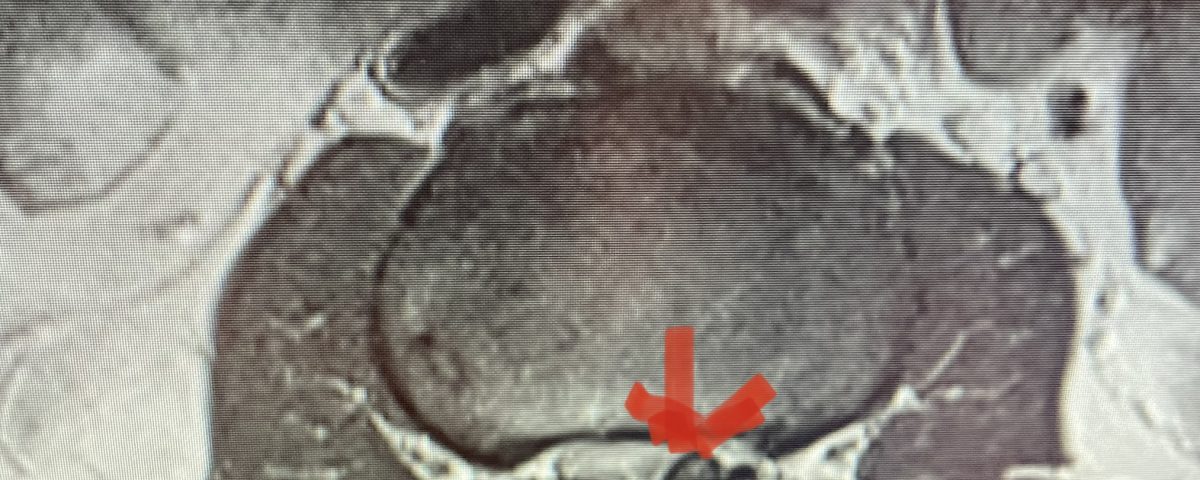
IMG 5280 5 1
Nervous tissue is soft. The thecal sac is surrounded by a rigid bony ring which forms the spinal canal. Any mass that fills the very small space of the spinal canal will cause the nervous structures to be deformed and hence may cause symptoms and signs. The spine when it develops arthritis in order to compensate for instability does not seem to know the nerves are present and does not care that the development of spinal stenosis or narrowing of the spinal canal and nerve tunnels will hurt the nerves.
There are different types of lumbar spinal stenosis that patients may develop. This includes central, lateral recess, and foraminal stenosis. Most people have a combination of these types. Central stenosis results in compression of the thecal sac by a variety of pathologies including thickened ligamentum flavum, facet hypertrophy, disc herniation, synovial cyst, or even a tumor.
Lateral recess stenosis typically involves compression of the nerve root as it takes off from the thecal sac, prior to entering the nerve foramen or tunnel. In lateral recess stenosis there is narrowing of less than 5 mm between the facet superior articulating process and the posterior vertebral margin and is bounded laterally by the pedicle. The nerve root gets caught medial to the pedicle. The nerve is compressed commonly from thickened ligamentum, short pedicles, or in particular an enlarged superior facet process which compresses the nerve as it descends prior to going underneath the pedicle in a region that is designated as the subarticular recess. (Figs 1, 2, and 3) With lateral recess stenosis, for example, of the L4-5 subarticular recess, the descending L5 nerve root will be compressed by the corresponding L5 superior facet. With foraminal stenosis the actual nerve root is compressed beyond the medial pedicular zone which can be caused by a far lateral type disc facet hypertrophy, tumor, or subluxation.

Figure 1: Axial lumbar spine images demonstrating the descent of the nerve root below the subarticular recess as it rounds the pedicle and enters the neural foramen. On the left shows the normal anatomy and on the right showing the descending nerve root being compressed in the lateral recess by a hypertrophied superior process with medial protrusion.
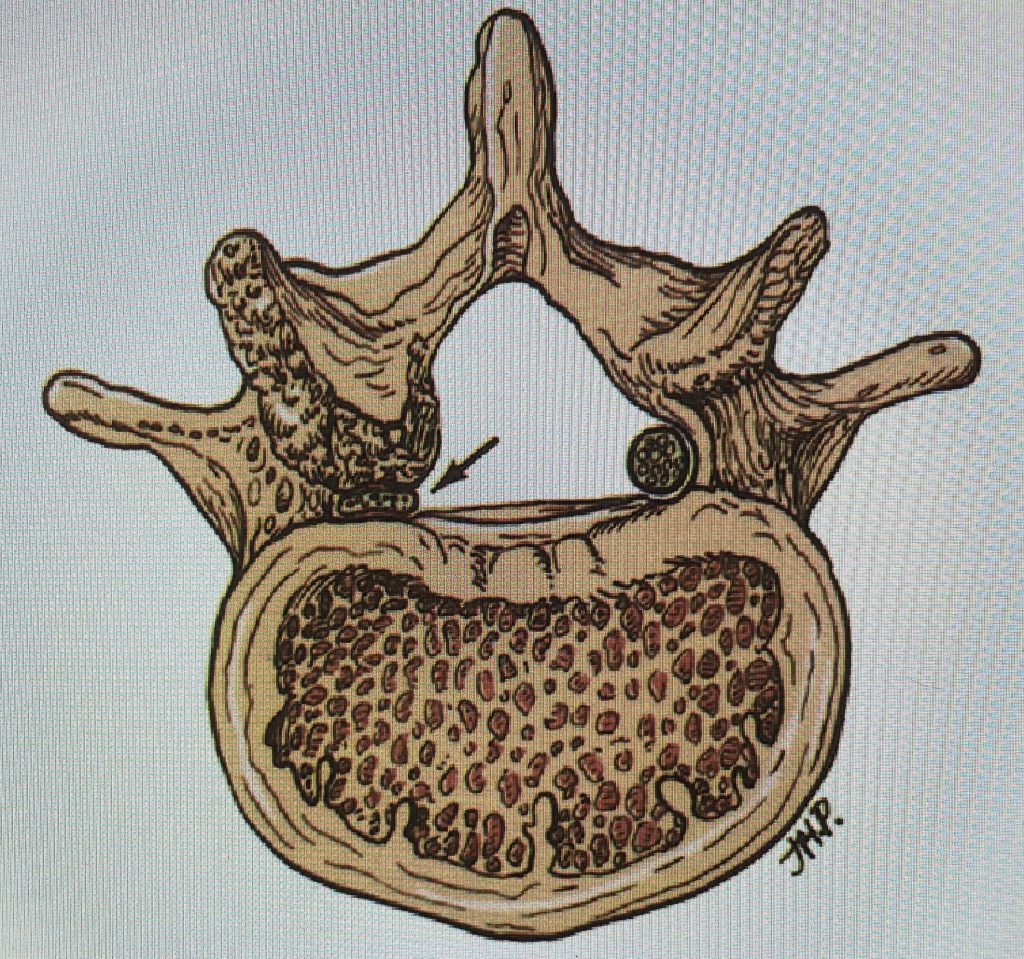
Figure 2: Cartoon axial image of the lumbar spine showing (arrow) severe narrowing of the lateral recess with flattening of the nerve root compared to a normal nerve root on the opposite side.
Symptoms can vary. Classic type symptoms of lumbar stenosis are pain in the back that radiates down the legs or into the buttocks that occurs when you stand or walk that is relieved when you sit, lean on a shopping cart, or ride a bike. When you are upright you extend your back and close down the spinal canal and the foramina. When you sit or flex you open up the spinal canal and foramina. Patients may have varying symptoms that may include heaviness, numbness or a feeling of weakness of their legs although objectively they usually have a normal neurological examination. Patients, however, sometimes if the lateral recess stenosis is quite severe will have weakness in that level of stenosis. For example a patient can have mild weakness of toe extension which is typical of L5 radiculopathy if they have a corresponding lateral recess stenosis at L4-5. When this objective finding occurs one is more confident that “this is the problem.” Patients with lateral recess stenosis can present with a unilateral radiculopathy that is dynamic, worsened by extending. This is in contradistinction to a patient with a herniated disc with radiculopathy that is often worsened by sitting.

Figure 3: Axial lumbar CT image demonstrating severely narrowed left lateral recess by a significantly hypertrophied facet joint (arrow) The lateral recess is formed by a triangle of the superior facet process, the pedicle, and the anterior margin of the vertebral body. Note the prominence and anterior protrusion of the superior facet process which is more anterior and medially oriented than the inferior process that comprises the facet joint.
Since patients with lateral recess stenosis usually have concurrent central stenosis they may just present with a preponderance of symptoms from their also present central stenosis. During a laminectomy or operation to remove the stenosis by shaving away the arthritic structures and thickened ligament causing the neural compression, the surgeon must attend to the lateral recesses just as importantly as the central space. The subarticular space is vital to decompress as the nerve descends past this as it rounds the pedicle out through the foramen which is below the descent which is typical for lateral recess stenosis. At the level of the foramen, the nerve may be compressed by a hypertrophied facet joint or disc that is protruded more laterally at the level of its corresponding foramen and compresses the superiorly positioned nerve root in that foramen. For example at the L4-5 level, the L4 nerve root will be compressed at the foramen whereas the thickened ligamentum in the subarticular recess or an enlarged L5 superior facet process that is more medial and intimately related to the subarticular recess will compress the descending L5 nerve root above its exit foramen. A patient with a far lateral L4-5 disc affecting the L4-5 foramen would typically develop an L4 syndrome with anterior thigh and shin pain versus a patient with a lateral recess syndrome of L4-5 where the pain will go down the back of the leg to the top of the foot in an L5 distribution as it is affecting the descending L5 nerve root PRIOR to exiting the lower foramen of L5-S1.
Here is a case that illustrates some of the points of lateral recess stenosis:
This 71 year-old male presents with a long history of progressive pain in the low back with radiation to both legs in the anterior thigh distribution, the left being worse than the right. He feels that his legs get weak. Standing and walking worsen the low back pain and lower extremity symptoms while sitting relieves the symptoms. He failed PT and epidural injections. Imaging studies revealed severe lateral recess stenosis do mainly to severed thickened ligament. He had severe lateral recess stenosis from L2-5 (Fig 4) as well as central stenosis. He also had a slight retrolisthesis at L3-4 and L4-5. He had on the left in particular a very enlarged protruded segment of thickened ligamentum in the subarticular recess at L3-4 (Fig 5) which was likely responsible for his left leg pain as the patient had symptoms of an L4-type syndrome. It was decided to perform a decompressive laminectomy from L2-5. Because of retrolisthesis it was decided to perform a noninstrumented onlay bone fusion or an in situ fusion from L3-5. In this case it was very important to decompress not only the thecal sac, but also the lateral recess with the thickened ligament at the point where the nerve makes its course into the forman. As a surgeon you must really undercut the facet joints to clear the lateral recess and feel how the nerve root with one’s instrument is being released as it enters the foramen. Postoperatively the patient had resolution of his leg pain, particularly on the left. In this case the most significant pathology was in the left L3-4 lateral recess, his symptoms and MRI findings correlated well which leads to the most successful operations.
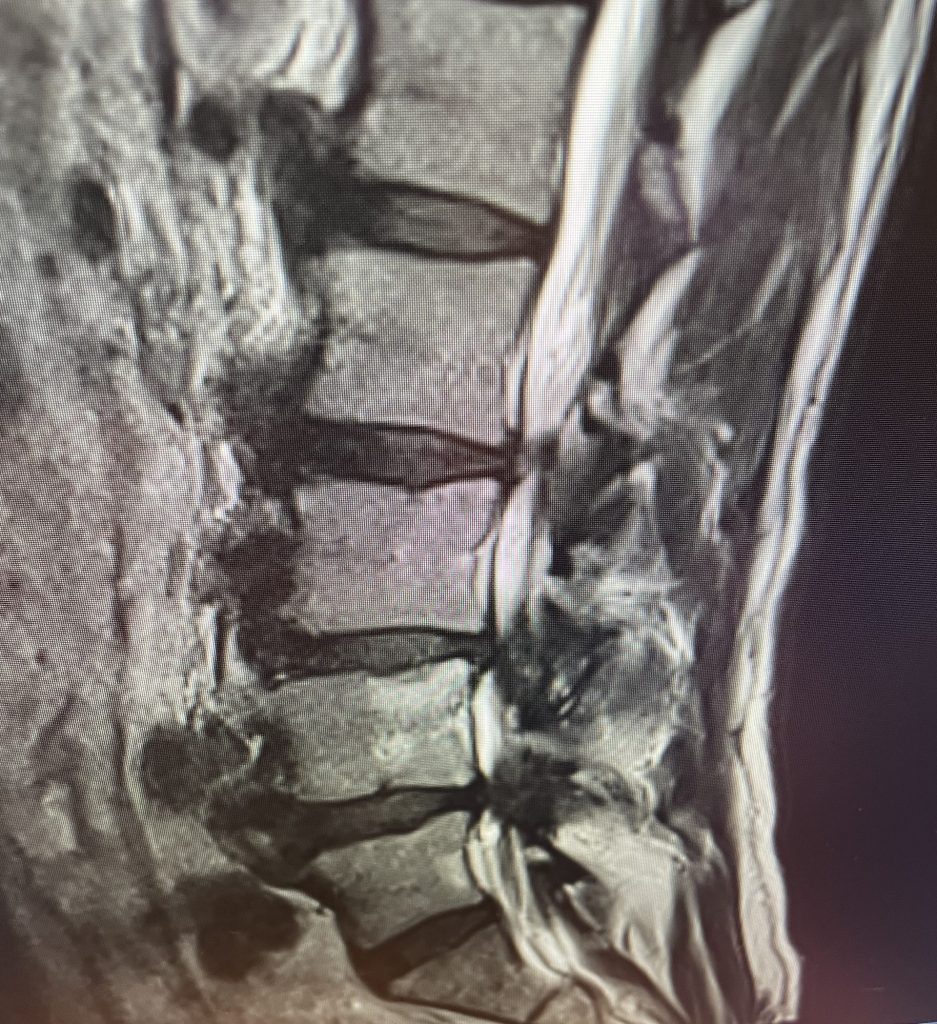
Figure 4: Sagittal T2-weighted MRI demonstrating severe lateral recess stenosis from L2-L5 as well as slight retrolisthesis at L3-4 and L4-5.

Figure 5: Axial T2-weighted MRI demonstrating severe bilateral lateral recess stenosis secondary to thickened ligamentum flavum. Notice the prominence of the left ligamentum in the subarticular recess.


