- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Lumbar Degenerative Scoliosis Case Study
Cervical Spinal Cord Compression With Myelopathy
April 26, 2022
Lumbar Stenosis
May 2, 2022
IMG 5061 scaled
Lumbar degenerative scoliosis is a tricky problem. In most cases, you are dealing with patients who are 65 and older who often present with concurrent medical issues, such as high blood pressure and diabetes. They are commonly on blood thinners for cardiac stents or atrial fibrillation. Patients in this age bracket are also quite spry these days because of modern medicine; and when surgery is presented to them, they generally only care about three things after surgery here on Long Island:
- When can I drive?
- When can I play golf?
- When can I have sex?
This speaks to the fact that these patients want to return to function and have a lot of future plans that they want to accomplish so you better come up with something good when making a plan and cannot discount their desires because of their age.
Degenerative lumbar scoliosis most commonly develops as a result of asymmetric degeneration of their lumbar spine. If a stack of disc spaces degenerates more on one side, then the spine will tend to curve. Sometimes one vertebra will slip to the side, or laterally, and cause the spine to tilt to one side. As a result of the degeneration and chronic instability, the patients very commonly have compensatory stenosis. Because of the lateral listhesis and degenerative asymmetric disc collapse with foraminal compromise, nerve roots will develop resultant up down compression and lateral stretch.
Young children will instead develop a curve because of a genetic predisposition, not because of degenerative processes. Occasionally, a patient with preexisting juvenile-type scoliosis will develop secondary degenerative changes. Patients may also have concurrent degenerative spondylolisthesis as well as the congenital variety at L5-S1. Surgically, the treatment fortunately encompasses both sets of issues. Patients will present with a variety of complaints including back pain, numbness, leg pain, and weakness. Patients more likely will develop chronic symptoms with an intact neurological exam. These patients are to be treated with conservative management including physical therapy, pain management, chiropractic care, and anti-inflammatory medication. Those patients who fail all means of conservative treatment, whose lifestyle is significantly affected or have a progressive neurological deficit, such as a foot drop, should be offered a surgical option. Patients with degenerative scoliosis often require a lumbar decompression because of concurrent central and foraminal stenosis. It is controversial whether a fusion should be offered because of the degree of auto-stabilization from arthritic changes. If a fusion is performed, it is sometimes the surgeon’s preference, age of the patient, concomitant spondylolisthesis or alignment, or degree of facet removal during a laminectomy that determines whether to perform an in situ or instrumented fusion.

Figure 1. AP lumbar x-ray demonstrating degenerative lumbar levoscoliosis with secondary arthritic changes.

Figure 2. T2-weighted sagittal and axial MRIs demonstrating severe L3-4 stenosis and an L5-S1 grade 1 spondylolisthesis and spondylolysis and L3-4 retrolisthesis. Note the anterior osteophyte formation at L2-3 with attempted autostabilization of segment.
This next Case Study illustrates many of these aforementioned concepts: This 65-year-old male presents with severe progressive low back pain and left leg pain for over a year. The patient also reported recent right leg pain as well. He stated that the bilateral leg pain was worse than his low back pain. Standing and walking made the pain worse. The patient had failed all means of conservative management including physical therapy, medications, chiropractic care, and injections.
He had mild proximal weakness of his hip flexors. He also had a history of diabetes, hypertension, and hypercholesterolemia. Imaging studies were obtained. Plain x-rays (Fig. 1) demonstrated a degenerative levoscoliosis with the apex of the curve at L2-3. Lumbar MRI (Fig. 2) showed severe degenerative disc disease with an L5-S1 grade 1 spondylolisthesis and a significant retrolisthesis at L3-4 with severe lumbar stenosis.
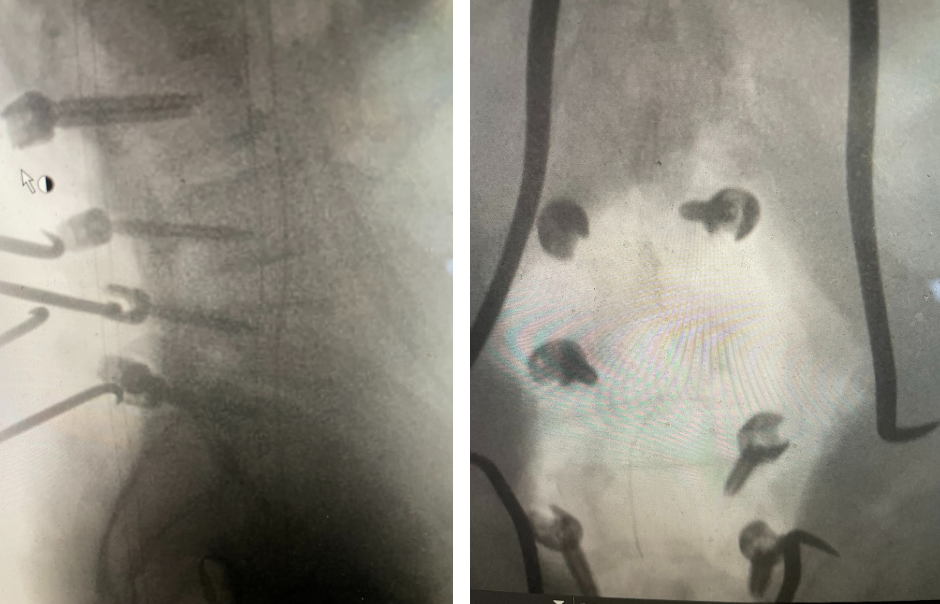
Figure 3. AP and lateral intraoperative fluoroscopic images demonstrating balanced pedicle screw placement.
We decided to perform a lumbar decompression L2-S1 with an instrumented fusion. The patient intraoperatively had severe thecal sac compression with severe facet arthropathy and thickened ligamentum flavum. The patient had bilateral L5 pars defects with a floating L5 lamina. Because of these factors and the patient’s age, it was decided to place screws (Fig. 3). The patient did well postoperatively with relief of his lower extremity pain and weakness.


