- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Lumbar Stenosis

Lumbar Degenerative Scoliosis Case Study
April 28, 2022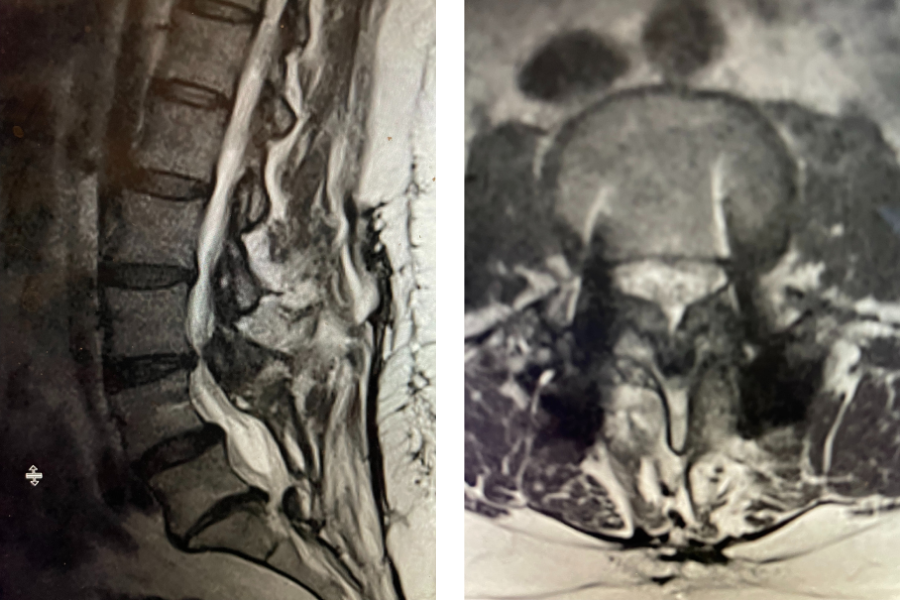
Severe Stenosis Above Prior Fusion
May 6, 2022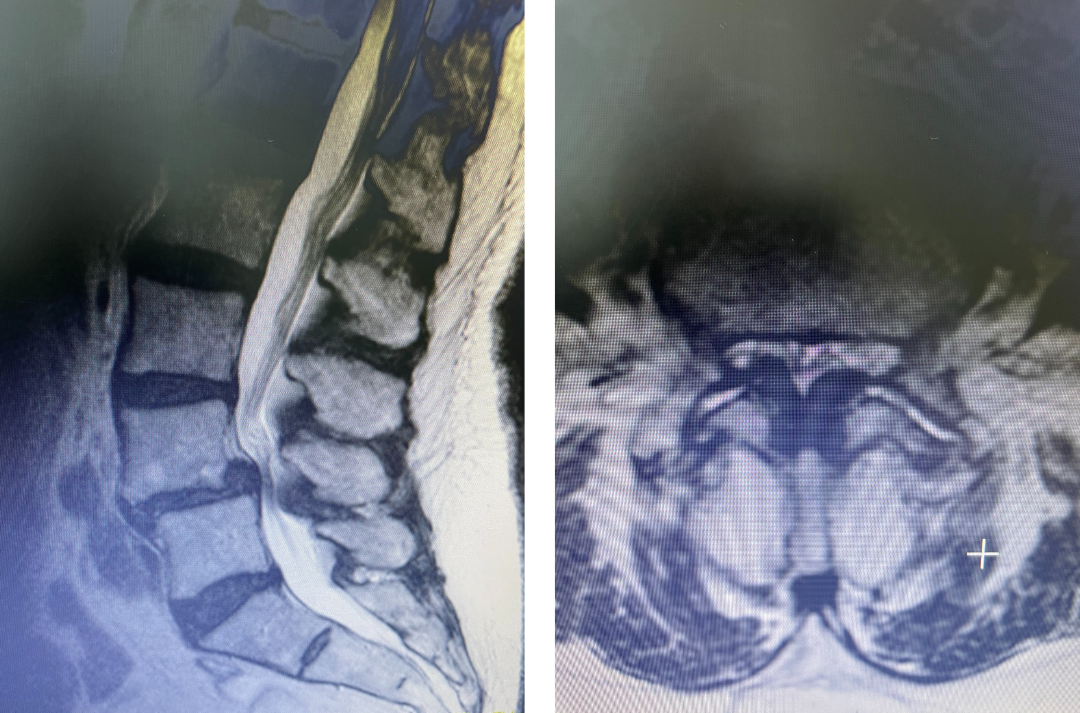
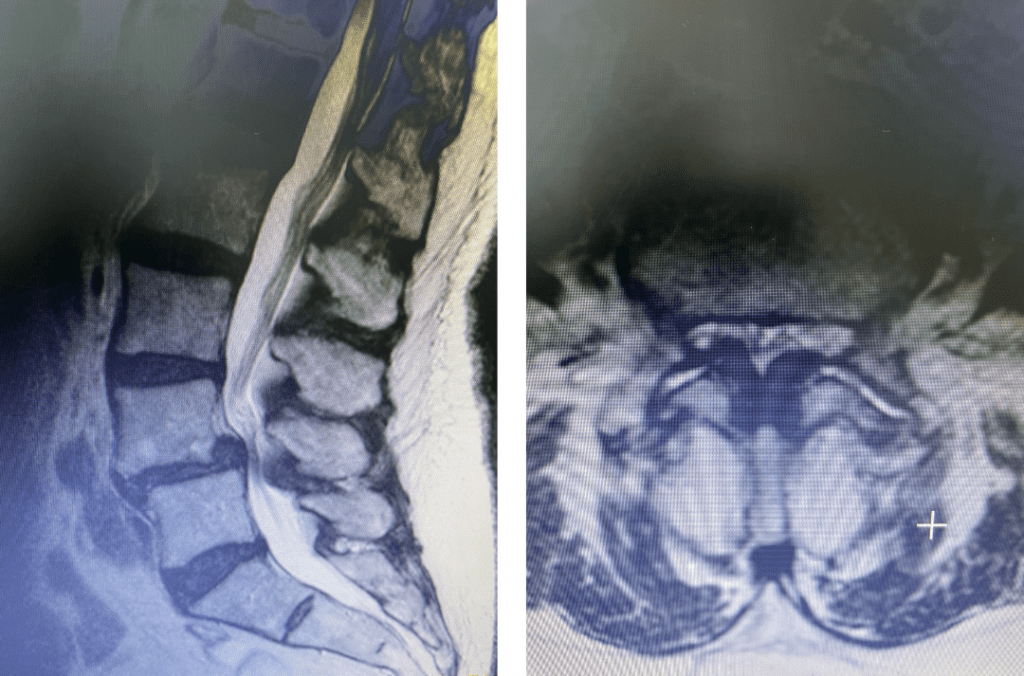
figure 1a and 1b lumbar stenosis
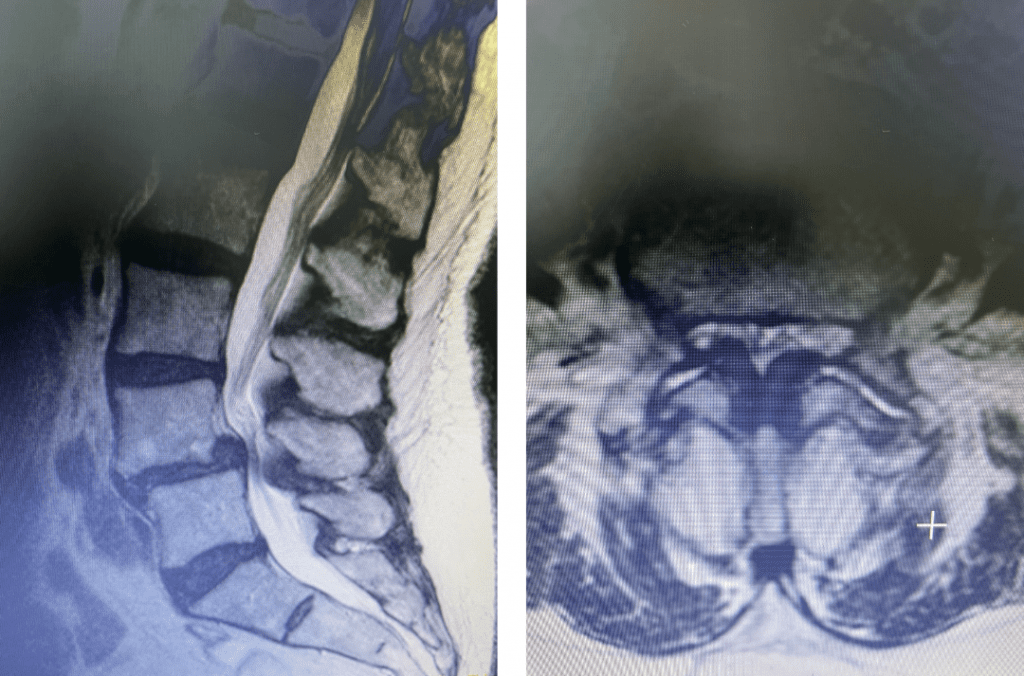
Figs 1a and 1b: T2 sagittal and axial lumbar MRI demonstrating severe L45 stenosis mainly secondary to thickened ligamentum flavum with a grade 1 spondylolisthesis at L45.
Lumbar stenosis is a fairly common condition I see in my office. Patients develop lumbar stenosis or narrowing of the spinal canal as a result of degenerative instability and laxity that is mainly age related. The body attempts to auto stabilize itself by forming stabilizing structures to compensate for instability such as thickening an already existing ligament or compensating by enlarging the facet joints which are the two regular joints on either side of the back of the spine in order to help improve stability. (Figs 1a and 1b) These structures are actually a form of arthritis and exert pressure on the canal in which the nerve sac travels through and the tunnel that the nerve leaves the spine. The spine does not know or care that the nerves are there and as a result the nerves get injured. The spine, at least the bony portion, is just taking care of itself. Patients are treated surgically for this by a procedure called a laminectomy which in essence restores the diameter of the spinal canal and the nerve tunnel by shaving away the arthritis. The trick of the laminectomy is to pick and dissect this sometimes soft and sometimes hard material from the nerve sac membrane for which it has been compressing for many years. Sometimes that material is really impaling the membrane which is called the dura. It is very important to do this gently in the manner in which we have been trained and avoid a tear or a leak in this membrane. This can happen and can be repaired with a stitch and some biological glue.
Patients sometimes require an additional fusion. This is the part of the procedure where we connect one spinal segment to the next by either using bone graft material or bone graft material using rigid fixation or pedicle screws. Because of the immobilization of the sometimes-painful spinal motion segment we are arresting the body’s signal to form compensatory arthritis and reformation of lumbar stenosis. In a more uncommon instance where a young person develops lumbar stenosis and has surgery, because of their longer lifespan and the fact that the signal to make arthritis has not gone away, it can be beneficial to add a fusion to prevent the reformation of stenosis. There are a number of other factors which lead to the decision to add a lumbar fusion to the laminectomy. For example, it is standard of care to perform a fusion in a patient who has a concurrent spondylolisthesis or slipped vertebra on another vertebra which can either be degenerative in nature or congenital. If we must extend the decompression out wider and take a good deal of the facet joint to more fully decompress a patient, we will augment the surgery to provide stability with a fusion. Interestingly the fusion part of the procedure is often for the spine surgeon the less technically demanding part of the procedure and quite safe. Most people do not perceive a change in their motion because not only does the patient compensate with the other motion segments, but also because of the improvement of their pain which was limiting their motion.
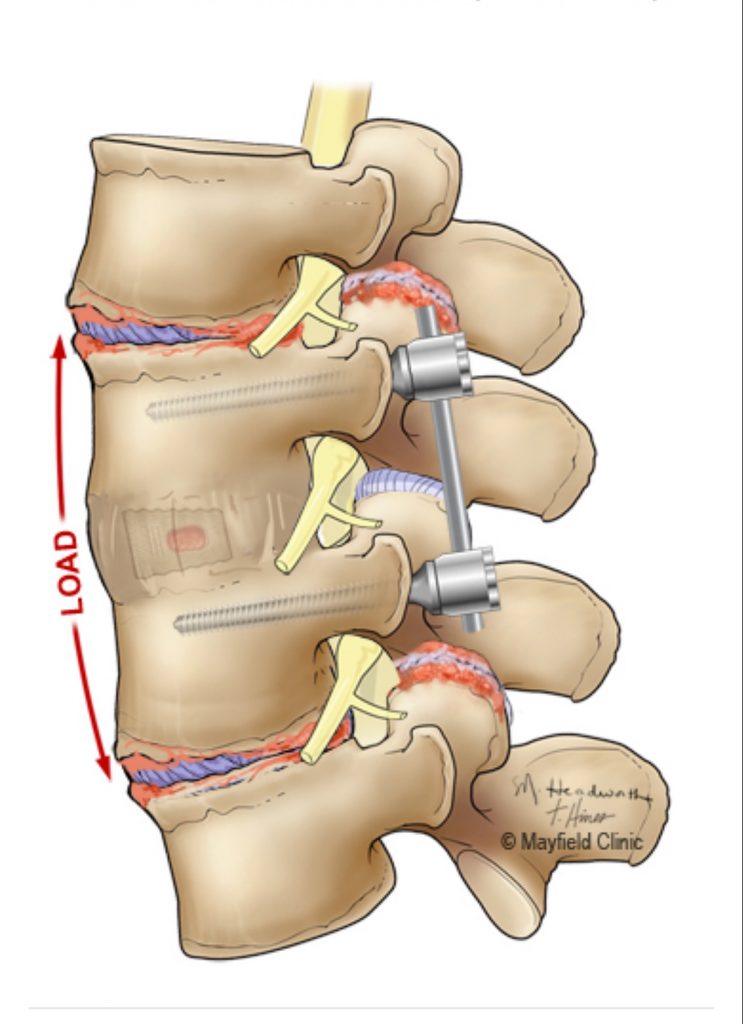
Fig 2. Illustration demonstrating the stresses and strains on the next lumbar segments, above and below.
Patients can sometimes develop a condition called Adjacent Segment Degeneration (ASD) after lumbar fusion. Sometimes patients can even develop this condition because one of their spinal segments will prematurely degenerate spontaneously and in essence “autofuse”; their disc degenerates to where it is bone on bone and not a functional or moveable spinal segment. When a spinal segment is immobilized, there is increased load on the adjacent level’s disc and facet joint which in turn cause abnormal motion and hence a resultant compensatory arthritis formation response which leads to lumbar stenosis (Fig 2). The incidence of patients who become clinically symptomatic from ASD varies from many studies from 2.5-18 percent. Patients who present with ASD can present on average 2-10 years from their initial fusion. When a patient presents with this they will often manifest symptoms that are familiar to them such as similar pain or numbness or weakness with or without back pain that they had when they originally presented to the neurosurgeon. We are in essence starting from the beginning with a new problem and a new level of disease. Therefore unless the patient has a progressive neurological deficit, we can again treat them conservatively with physical therapy, chiropractic care, anti inflammatories, acupuncture, and epidural injections. Again, if the patient fails these measures then surgery may be indicated to address the new level of concern. It is very important for that new level of concern to correlate with the patient’s symptoms. Here we will show a case of ASD which eventually came to surgery:
This 72 year old female had a long history of low back pain, leg pain, and scoliosis for which ten years ago she had a lumbar laminectomy followed by an instrumented L4-S1 fusion a year later. Since that time she had progressive low back pain and right lower extremity, weakness, and numbness. She presented with her leg symptoms being the biggest problem. MRI demonstrated a degenerative scoliosis with severe stenosis above the L4-S1 laminectomy and instrumented fusion. She had severe L2-3 and L3-4 stenosis. (Figs.3a,3b,3c 3d). After failing conservative management, she underwent an L2-L4 revision laminectomy and in situ fusion. She did well postoperatively. Considerations in performing a revision spine surgery is scar formation which initially makes it challenging to identify landmarks even in the region above that was not previously operated on. And of course during the dissection of compressive material on the dura, it is difficult to identify planes of separation and therefore an increased risk of a CSF leak. It was felt because of the severity of the scoliosis and her age we augmented the laminectomy with an in situ fusion, or a fusion with just bone graft without instrumentation. It is controversial whether a fusion is actually necessary in the case of a stable degenerative scoliosis with stenosis but the accepted approach is to perform a fusion If an instrumented fusion is considered it would require at least a T11-pelvis fusion. Since we performed only a 2 level laminectomy with a severely osteophytic spine, we compromised with an in situ fusion, reducing blood loss, operating time, and risk for infection. Because of the degree of spondylotic disease as a result of the stresses and strains on the spine given the scoliosis, the spine attempts to auto stabilize by forming these buttresses of arthritic material.
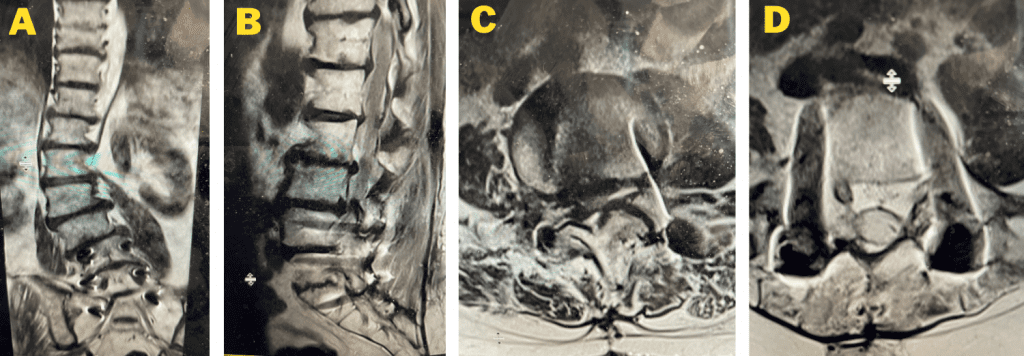
Fig 3a: Coronal T2-weighted MRI demonstrating significant detro lumbar degenerative scoliosis with a prior L4-S1 instrumented fusion. Note lateral listhesis of the L3-4; Figs 3b and 3c: Sagittal and axial T2- weighted MRIs showing severe lumbar stenosis above the prior L4-S1 fusion; Fig 3d showing an axial image T2-weighted MRI at the level of the prior L4-5 portion of the fusion showing no recurrent stenosis