- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Severe Stenosis Above Prior Fusion
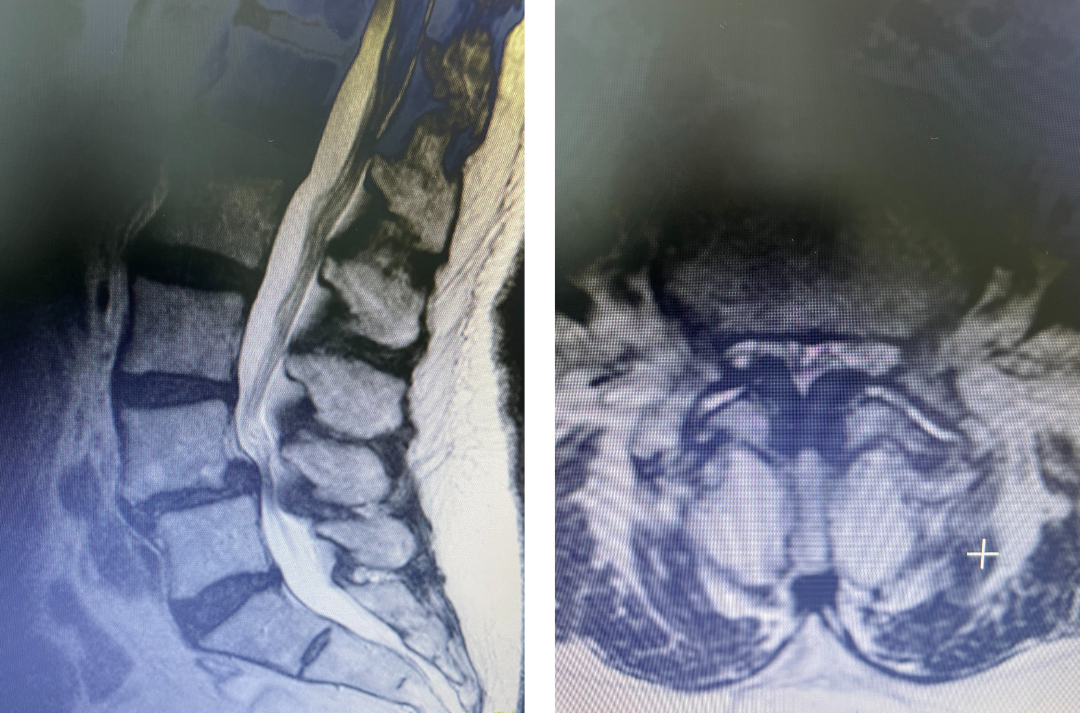
Lumbar Stenosis
May 2, 2022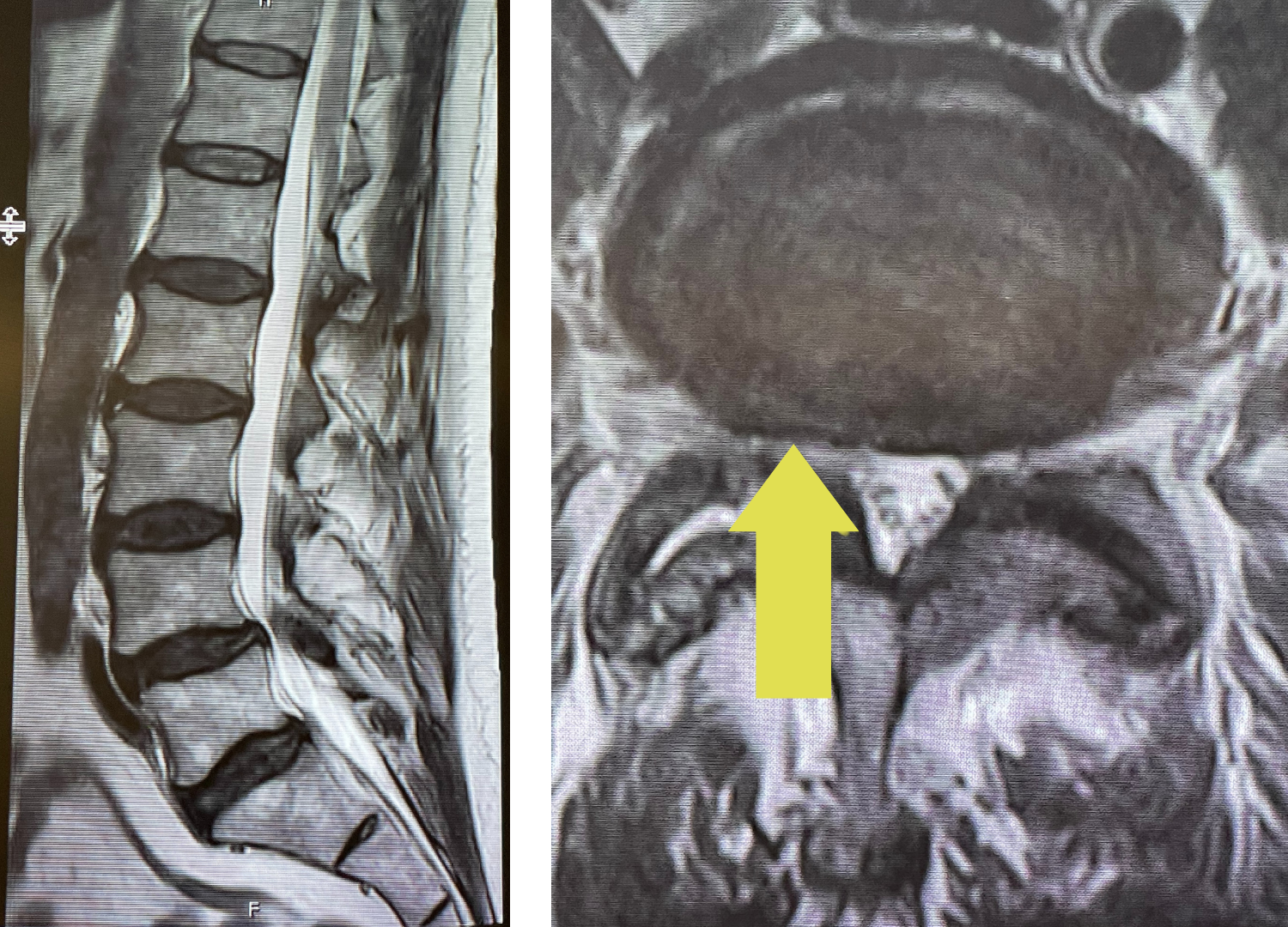
Grade 1 Spondylolisthesis At L4-5 With Severe Lumbar Stenosis
May 9, 2022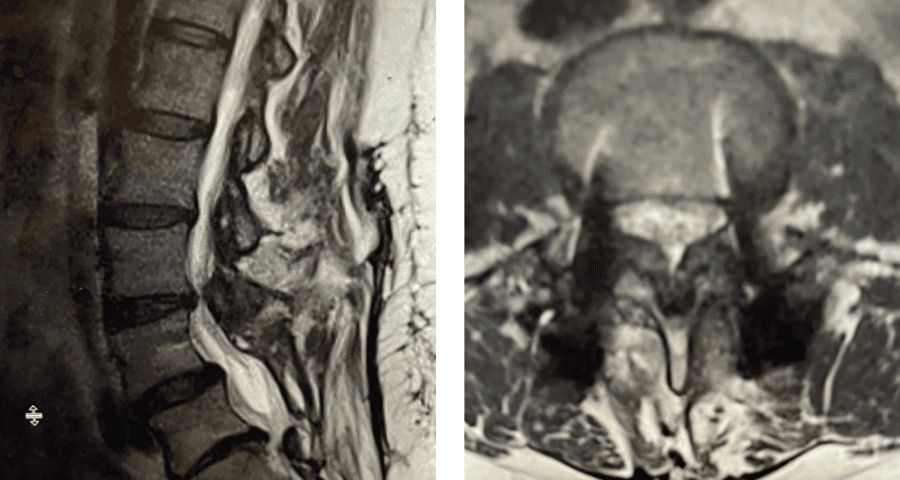
Figure 4 5 4
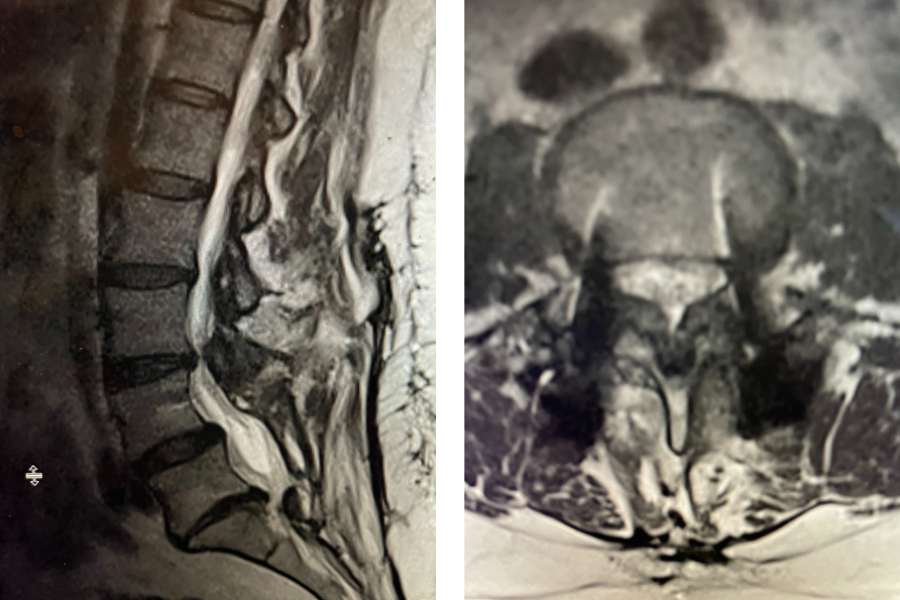
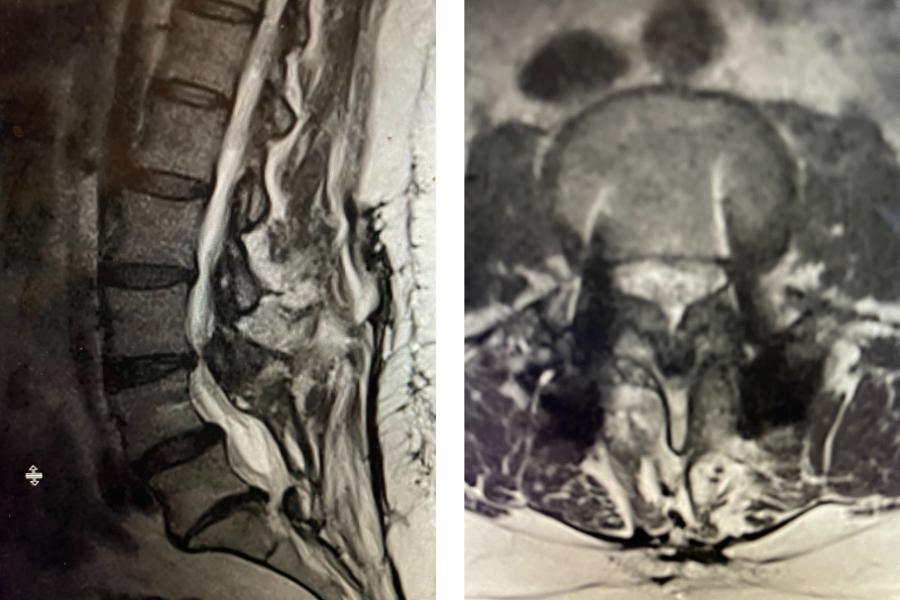
Figure 1. Sagittal and axial T2-weighted MRI of the spine demonstrating severe next segment stenosis above the prior fusion worse at L3-4 mainly due to severe ligamentous hypertrophy
This next patient was a 54-year-old female who had a long history of low back pain with radiation to both legs. She had a prior L4-S1 instrumented fusion and a L3-S1 laminectomy two years prior. In the past six months she has developed worsening low back pain and bilateral leg radiation. She had tried medications, epidurals, and PT but with no improvement. Imaging revealed severe stenosis above her prior fusion at L3-4 secondary to thickened ligament and facet hypertrophy or enlargement. This was also evident slightly less so at L2-3 (Fig 1). This ligament is in particular commonly involved in causing lumbar stenosis. This is a ligament that looks yellow in the operating room for which its purpose normally is to act like a rubber band to limit extremes of flexion and to aid in upright posture. Perhaps this ligament thickens to compensate for the decrease in upright support as we get older. It was decided initially to perform an L2-4 revision laminectomy, explore the prior fusion, and remove the hardware. We would leave the L4 screws in and add screws at L2 and L3, giving her a shorter segment of fusion mass if she was indeed fully fused.
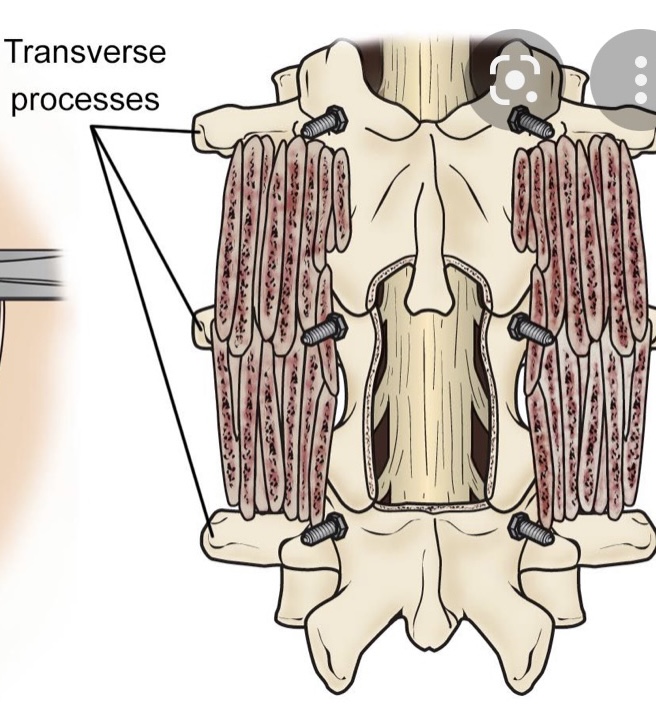
Figure 2. Illustration demonstrating an example of a lumbar In Situ fusion with bone graft material placed on top of transverse processes
At the time of surgery, it was noted that she had not only a very solid L4-S1 fusion but also her hardware was 100% encased in the bone. It was so much so that we decided not to remove this bone as we felt it would cause excess blood loss and perhaps add risk to neurological injury because of the force sometimes necessary to essentially “chisel” out this bone. We decided as a compromise, given her relatively young age and risk of redeveloping stenosis in the future, was to perform an “in situ” fusion from L2 to the top of the prior L4 fusion mass. It is to be remembered that the signal to form lumbar stenosis does not disappear once a laminectomy is performed, and a fusion prevents that signal. An “in situ” fusion is one where bone graft material is placed on the sides of the spine along bony extensions called transverse processes (Fig 2). The purpose of these processes besides serving as an excellent scaffold for bone graft material they also attach the back muscles or “paraspinal muscles” that allows a side or lateral bending motion or twisting. This way the patient will have reasonable stability after the bone consolidates and fuses. It has been found that a patient may not have to, with an in-situ fusion, have it be perfectly solid for it to serve the purpose of providing stability. The patient had an uneventful postoperative course.