- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Severe Stenosis With A Grade 1 Spondylolisthesis

NSPC Mobile Patient
May 10, 2022
Spinal Cord Compression In Obese Patient
May 11, 2022
IMG 5185 scaled
This week was frantically filled with interesting spine cases that illustrate important biomechanical principles and important common problems that we face as neurosurgeons.
The first was a 64-year-old male with progressive low back pain with severe left lower extremity pain. When the patient came to the office, he was very uncomfortable. His leg symptoms were worse than his low back pain. He had tried conservative management including epidurals and chiropractic care.

Figure 1. Sagittal T2-weighted MRI demonstrating severe L2-4 stenosis and slight grade 1 spondylolisthesis L3-4.
Figure 2. Axial T2-weighted MRI demonstrating severe concentric stenosis at L3-4 due to severely enlarged facet joints and ligamentous hypertrophy
MRI demonstrated severe L3-4 stenosis with a grade 1 spondylolisthesis. He also had L2-3 stenosis. (Fig 1). On axial MRI (Fig 2) he had severe concentric stenosis at L3-4, but on careful examination it appeared that the right side had particular distortion of the anterior aspect of the thecal sac, perhaps secondary to a facet cyst. It seemed more likely coming off the facet joint and not a disc herniation. Although the right side was worse, most of his symptoms were on the left. Why does that happen? I don’t have a great explanation. Clearly the left side is also compressed but sometimes the body just chooses the side to be affected symptomatically when both sides are involved. This is true for compression of the spinal cord for instance in the cervical spine. What is not right, however, is that if a patient has a lateralized disc herniation and the opposite side is symptomatic and without compression, then one should not offer surgical treatment unless that disc is causing severe compression on one side with just less compression on the ipsilateral symptomatic side. Then one can argue that the pathology is having an effect on the opposite side if there is some degree of bilateral compression even if the ipsilateral symptomatic side is less compressed.
We elected to perform a decompression from L2-L4. Because the patient had a spondylolisthesis at L3-4
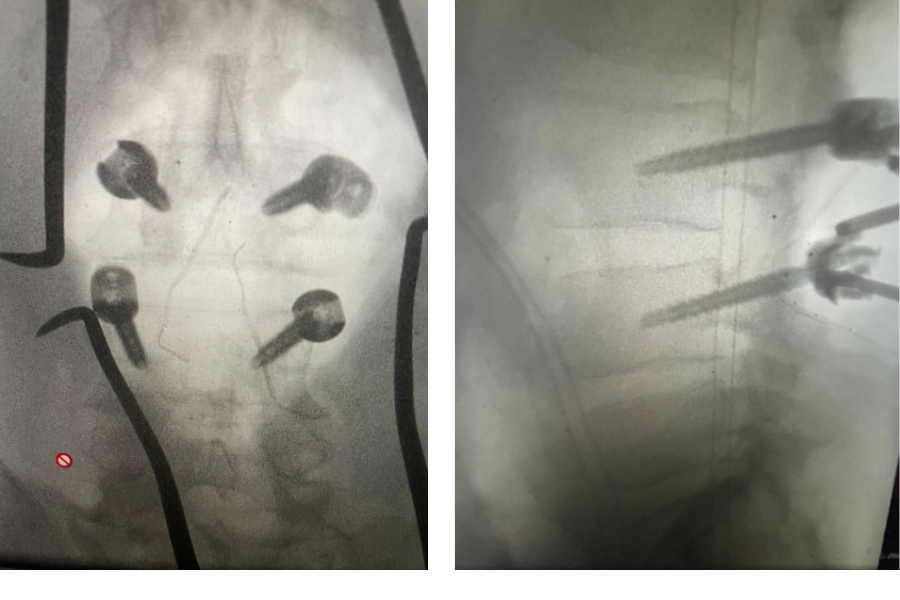
Figure 3. Lateral and AP lumbar intraoperative fluoroscopic images after pedicle screw placement for L3-4 fusion
we augmented our decompression with an instrumented fusion at that level, particularly because of the degree of facet joint removal to adequately decompress him (Fig 3). The facet joints were very overgrown and because of that just undercutting the facet would not prove adequate. These facet joints are enlarged because the patient had degeneration of the cartilage and ligaments of the joints, disc space and supporting structures. A common occurrence is for the spinal segment to slip or “listhes” in Greek. In order to compensate for this instability, the body tries to compensate and enlarges what it has available like the joints and the ligaments. In doing so the spine paradoxically hurts itself in creating spinal stenosis. The bone really does not communicate with the nerve sac and therefore the sac is squeezed because of these enlarged structures. The patient did well postoperatively with relief of his left leg pain and ambulated the same day of his surgery.
In the case of a spondylolisthesis, it has been well studied that the addition of a fusion in degenerative spondylolisthesis, either instrumented or non-instrumented, improves functional outcome. Improved stability to improve back pain is one factor, but in addition by performing a fusion you arrest the signal to enlarge the joints or thicken the ligaments to compensate for the instability which are compressive structures. This structure formation is what arthritis is.