- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
When Just Enough is Enough
NSPC Neurosurgeon Dr. Michael Brisman Authors Brain Surgery Textbook
January 4, 2024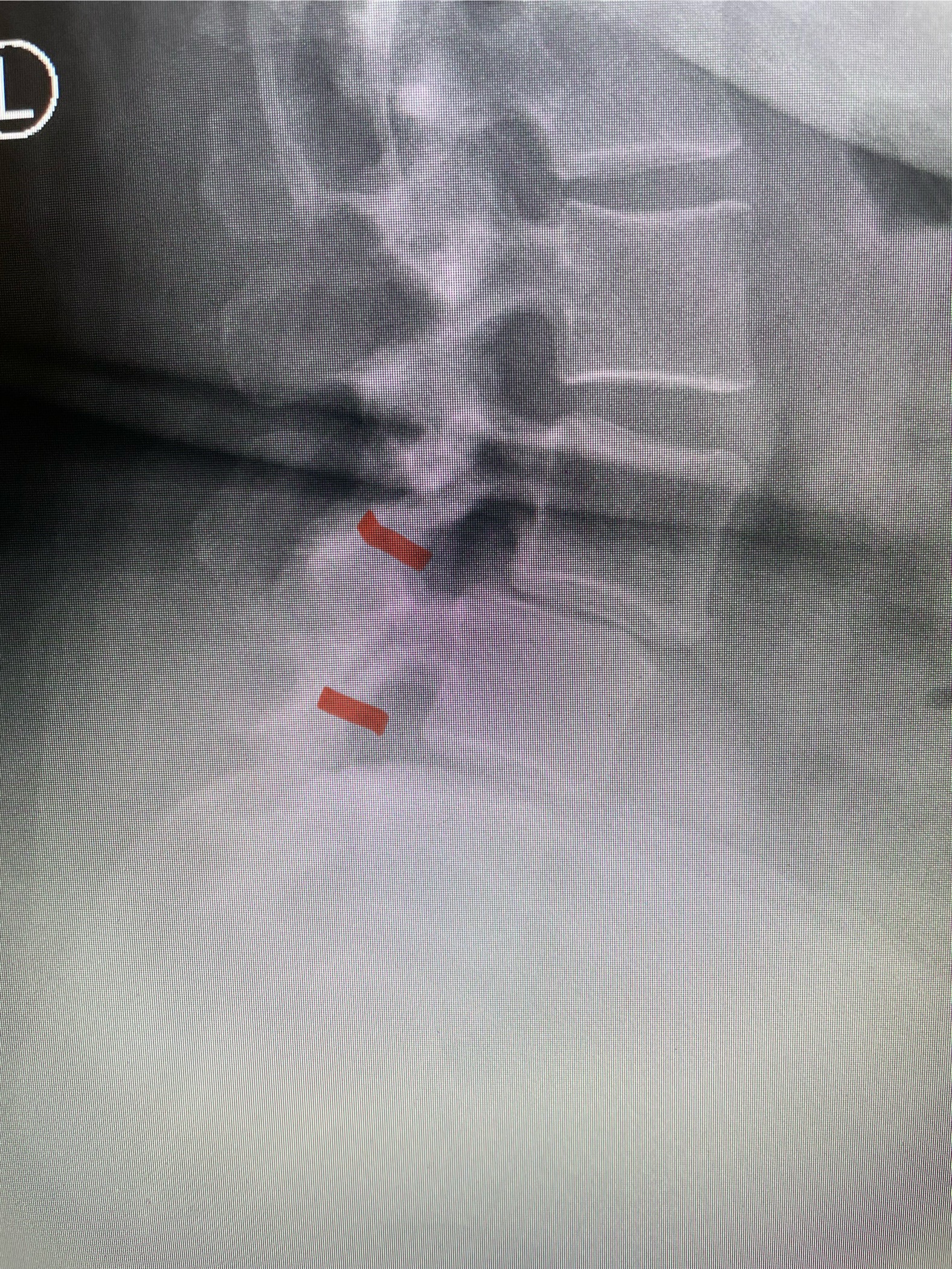
LUMBAR SURGERY CAN BE DONE IN THE MORBIDLY OBESE PATIENT
February 27, 2024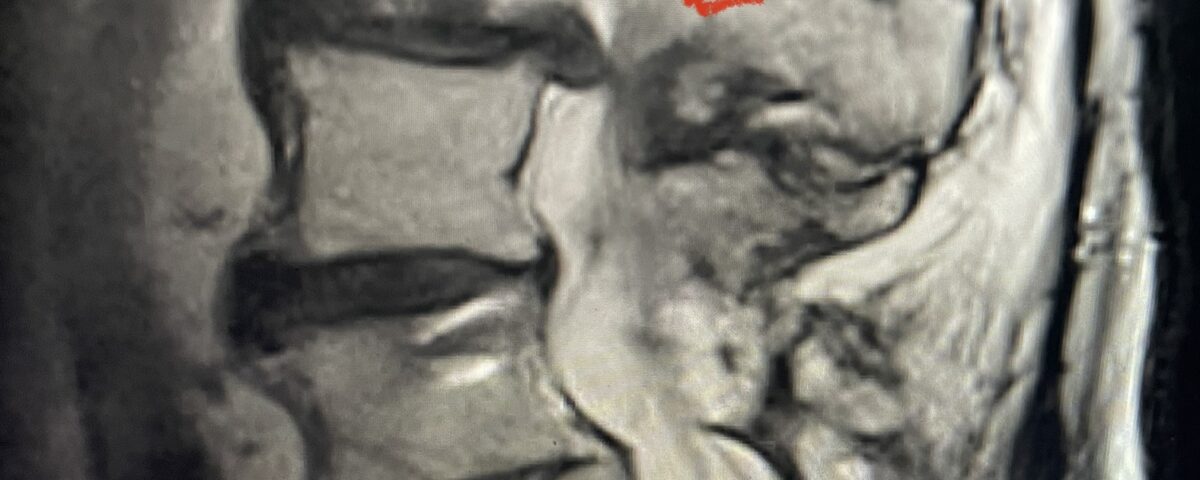
We as spine surgeons can sometimes change our approach in the preoperative planning of a patient’s surgery. Sometimes an approach that is so initially obvious becomes modified as one considers the patient’s underlying medical condition.
In patients who have lumbar spinal stenosis and significant cardio/pulmonary conditions, surgery is the last resort. However, some patients with these conditions may fail all means of conservative management where surgery becomes their only option for relief. In those patients, one should strive to do the least complex surgery that is necessary to get the job done for them. In this case study, we are confronted with a new problem in a 78 year-old male patient that was in poor medical condition who had had two prior lumbar laminectomies with resultant fusion and instrumentation from L4-S1. There was now retrolisthesis of L2-3 with severe stenosis (Fig.1)

Fig 1a: Sagittal T2 weighted lumbar MRI demonstrating severe L2-3 stenosis (red arrow)
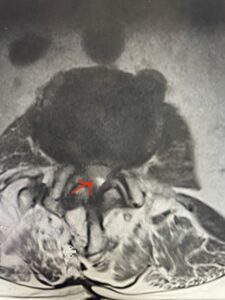
Fig 1b: axial T2-weighted MRI demonstrating severe lumbar stenosis (red arrow)
The patient had severe low back pain and severe pain that radiated to the right hip and thigh worse with standing and walking. The leg pain was worse than the back pain. He also had complaints of weakness of his legs for which if he stood too long, he would lose his balance. He also could not negotiate stairs with his right leg. Patient had 4 ⁄ 5 weakness of his right hip flexor.
The patient had failed all means of conservative management including Physical Therapy and epidurals. He had an extensive medical history including stroke, cardiac stents, diabetes on insulin, hypertension, hypercholesterolemia, and kidney disease. Since he had a prior fusion with instrumentation for L4-S1, it was interesting that the patient had not developed significant next segment stenosis at L3-4. However, CT analysis (Fig. 2) demonstrated a partial fusion that extended from L3 to L4 which prevented abnormal motion.

Fig 2: Coronal lumbar CT demonstrating L4-S1 fusion with instrumentation with some incomplete bony fusion to the L3-4 segment (red arrow)
Initially on first analysis we reflexively planned to remove the prior instrumentation and extend the fusion to L2 with new instrumentation as well as a decompressive laminectomy at L2-3. This obviously in a revision case would add significant operative time even prior to commencing the decompression at L2-3 to relieve the leg pain which was the most significant problem for the patient. Taking into account his poor medical condition we felt there could be another approach that would decrease operative time but solve the most disabling problem which was the leg pain. We elected to do an L2-3 revision laminectomy and perform only an insitu fusion from L2-4, leaving the hardware alone.
Surgery was quick and the patient was able recover quite well without leg pain. I am glad we made a lesser approach. Patients mainly can live with back pain much more than terrible leg pain. This case to me illustrates the concept of less is more in a patient with a complex medical history. It is better to hit a triple in an older or sicker patient.



