- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Carotid Cavernous Fistula (CCF) Study
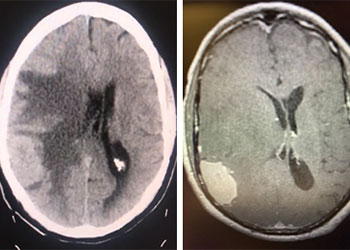
Atypical Convexity Meningioma
October 27, 2021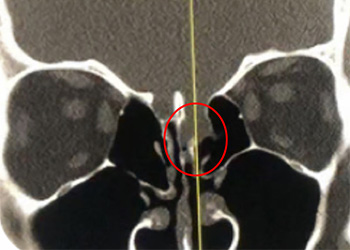
39 year old physician with rhinorrhea and an encephalocele
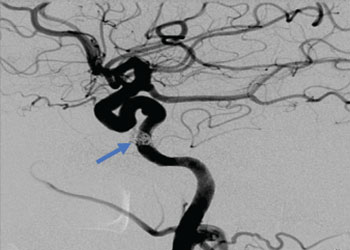
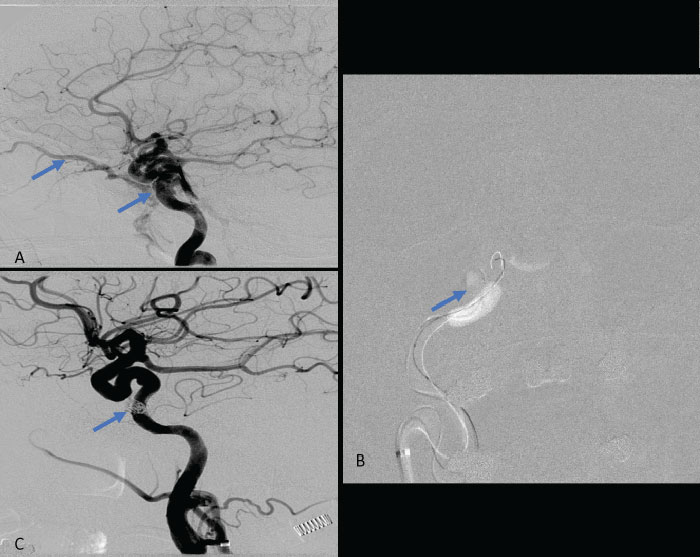
January 17, 2022Collateral venous drainage into the orbit and skull base was observed (Fig. A). After successful cannulation of the direct aperture between the right carotid artery and the cavernous sinus, balloon-assisted coil embolization of the posterolateral compartment was performed until the fistula was closed (Fig. B and C). She experienced immediate cessation of her pulsatile tinnitus with the early improvement of the right VI nerve palsy and near-complete recovery of her vision within 6 weeks.
Figure: (A) Right ICA Cavernous Fistula with Venous Shunting (B) Balloon Assisted Coil Embolization (C) Fistula Cured Post Embolization
Key Learning Points:
- Carotid-Cavernous Sinus Fistula (CCF) may occur because of traumatic or spontaneous communication in the walls of the intra-cavernous ICA or its branches directly to the cavernous sinus resulting in short-circuiting or shunting of high-pressure arterial blood into the venous system of the cavernous sinuses.
- Intra-cavernous aneurysms are often felt to predispose to a Direct CCF which have high rates of arterialized blood flow and can result in rapid progression of clinical symptoms including cranial nerve injury and vision loss.
- Early evaluation by a neurovascular specialist is recommended for patients presenting with new-onset or progressive pulsatile tinnitus, especially in patients with associated visual symptoms or new neurologic deficits.
CATEGORY: ENDOVASCULAR // CAROTID CAVERNOUS FISTULA (CCF)
Carotid Cavernous Fistula (CCF)
A 61-year-old woman who is otherwise healthy presented to her PCP with progressive right-sided pulsatile tinnitus for 4-6 weeks. Her PCP and ENT evaluated her extensively and prescribed multiple courses of steroids and subsequent unremarkable MRI and MRA imaging. She developed acute onset diplopia secondary to a new partial right VI nerve palsy several days prior to our evaluation. A cerebral angiogram confirmed the presence of a high flow direct fistula of the right internal carotid artery–right cavernous sinus.