- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Hemangioblastoma
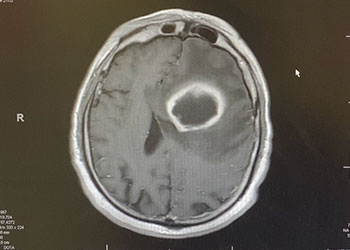
50 year old man with new onset aphasia and a left frontal mass / Brain Abscess
October 27, 2021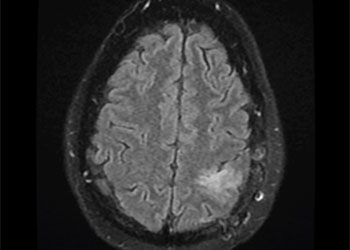
Grade II Oligodendroglioma
October 27, 2021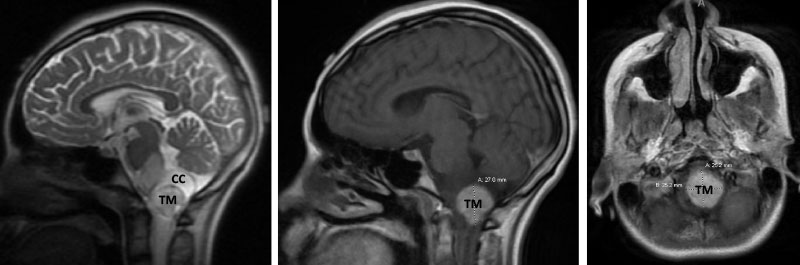
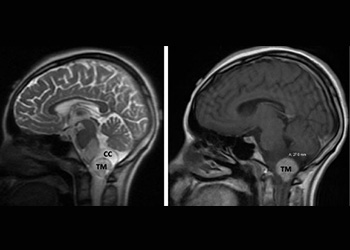
Figure 1. Brain MRI showing tumor mass (TM) with cystic component (CC) and edema (T2-weighted MRI, left) in the lower brainstem and upper cervical cord. Mass with contrast enhancement (post-contrast T1-weighted MRI, middle and right).
A teenage boy presented with 6 months of weight loss and difficulty swallowing. A contrast-enhancing mass in the brainstem and upper cervical cord was found which was suspicious of a symptomatic hemangioblastoma (Figure 1).
A pre-surgical cerebral angiogram was performed to investigate the vascular lesion and to attempt pre-operative embolization (Figure 2). A hypervascular posterior fossa tumor mass was confirmed with major vascular supply from the anterior spinal artery. The attempts for pre-surgical embolization were difficult (anterior spinal artery access) and had to be aborted.

Figure 2. Posterior circulation cerebral angiogram. Right vertebral artery (R-VA) injection, mid- and late-arterial phase (A, B) and left VA injection mid- and late-arterial phase (C, D) showing filling of a vascular tumor mass (TM) fed by the anterior spinal artery (ASA). Basilar artery (BA).
Following, the intramedullary brainstem tumor was successfully resected via suboccipital craniotomy and upper cervical laminectomy. The patient did well after surgery.
Five years following surgery, the patient is fully recovered, and is a thriving high school senior.
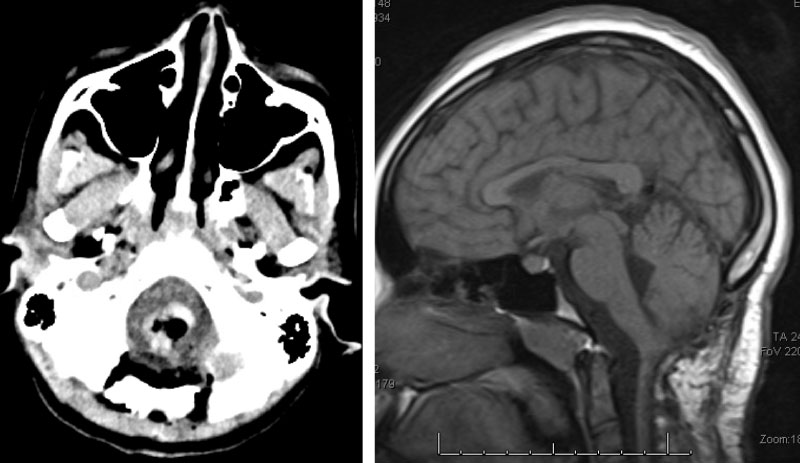
Figure 3. Immediate post-op CT (left) and two-year follow-up MRI (right).
Treatment Considerations:
Hemangioblastoma of the brain and spinal cord are rare, sporadic, and benign vascular tumors most commonly arising from the cerebellum1,2,3. An association with vonHippel-Lindau disease exists which is inherited in an autosomal-dominant manner4.
Symptoms from the slowly growing tumor stem from mass effect caused by the cystic component and the tumor. Contrast-enhanced brain MRI shows a hypervascular tumor. However, the exact location of the tumor in terms of intra- or extramedullary or intraand extramedullary can be difficult to determine on imaging and may only be clarified during surgery5.
Traditionally, surgical resection has been the treatment of choice 2,3. Pre-surgical embolization and stereotactic radiosurgery have also been used, albeit a systematic approach has been difficult to realize due to the rare nature of the disease 6,7.
REFERENCES:
- Nguyen HS, Doan N, Gelsomino M, et al. Intracranial hemangioblastoma – a SEER-based analysis 2004- 2013. Oncotarget 2018; 9: 28009-015.https://www.oncotarget.com/article/25534/text/
- Yin X, Li C, Li L, Duan H. Safety and efficacy of surgical treatment for brainstem hemangioblastoma: a metaanalysis. Neurosurg Rev. 2020 Apr 30. doi: 10.1007/s10143-020-01305-https://link.springer.com/article/10.1007/s10143-020-01305-3
- Epub ahead of print. PMID: 32356022. 3. Giammattei L, Messerer M, Aghakhani N, et al. Surgical resection of medulla oblongata hemangioblastomas: outcome and complications. Acta Neurochir (Wien) 2016; 158: 1333-41. https://pubmed.ncbi.nlm.nih.gov/27185165/
- Lonser RR, Glenn GM, Walther M, et al. von Hippel-Lindau disease. Lancet. 2003;361:2059–67. https://www.sciencedirect.com/science/article/abs/pii/S0140673603136434
- Imagama S, Ito Z, Wakao N, et al. Differentiation of localization of spinal hemangioblastomas based on imaging and pathological findings. Eur Spine J 2001; 20: 1377-84. https://link.springer.com/article/10.1007/s00586-011-1814-6
- Bridges KJ, Jaboin JJ, Kubicky CD, Than KD. Stereotactic radiosurgery versus surgical resection for spinal hemangioblastoma: A systematic review. Clin Neurol Neurosurg. 2017; 154: 59-66. https://www.sciencedirect.com/science/article/abs/pii/S0303846717300124
- Sakamoto N, Ishikawa E, Nakai Y, et al. Preoperative endovascular embolization for hemangioblastoma in the posterior fossa. Neurol Med Chir (Tokyo) 2012; 52: 878-84. READ MORE Man develops mild dizziness, headache after incidental trauma. https://www.jstage.jst.go.jp/article/nmc/52/12/52_3092/_article/-char/ja/
CATEGORY: ENDOVASCULAR // HEMANGIOBLASTOMA
Hemangioblastoma