- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Laminectomy and Fusion Solves Decades of Back Pain

Pituitary Tumor with Cushing’s Disease
October 27, 2021
50 year old man with new onset aphasia and a left frontal mass / Brain Abscess
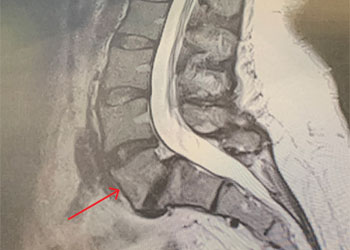
October 27, 2021MRI of the lumbar spine (Fig. 1) demonstrated a grade 1-2 spondylolisthesis at L5-S1 with bilateral pars defects with significant L5-S1 foraminal compression. She had an associated L4-5 retrolisthesis with secondary degenerative changes with a dysmorphic trapezoidal L5 vertebral body.
The patient underwent a decompressive laminectomy from L4-S1 with decompression of the L5 nerve roots and instrumented L4-S1 fusion (Figs. 2 and 3). Intraoperatively she had a very loose L5 lamina and had thickened degenerative ligamentous material severely flattening the L5 nerve roots at the level of the lysis defect. The patient tolerated surgery well with significant relief of back and leg pain.

Figure 1: Sagittal MRI T2-Weighted image of lumbar spine demonstrating grade 1 L5-S1 spondylolisthesis and retrolisthesis of L4-5 with significant degenerative disease of both segments. Note dysmorphic L5 vertebral body (arrow).
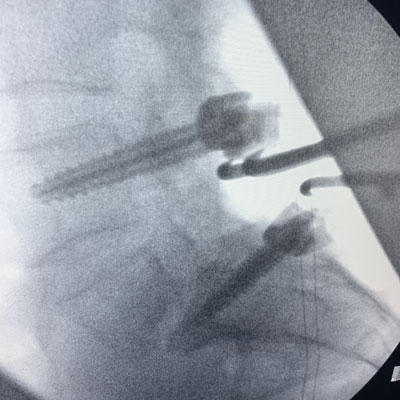
Figure 2 – Fluoroscopic sagittal and AP images demonstrating post-pedicle screw placement at L4 and S1.
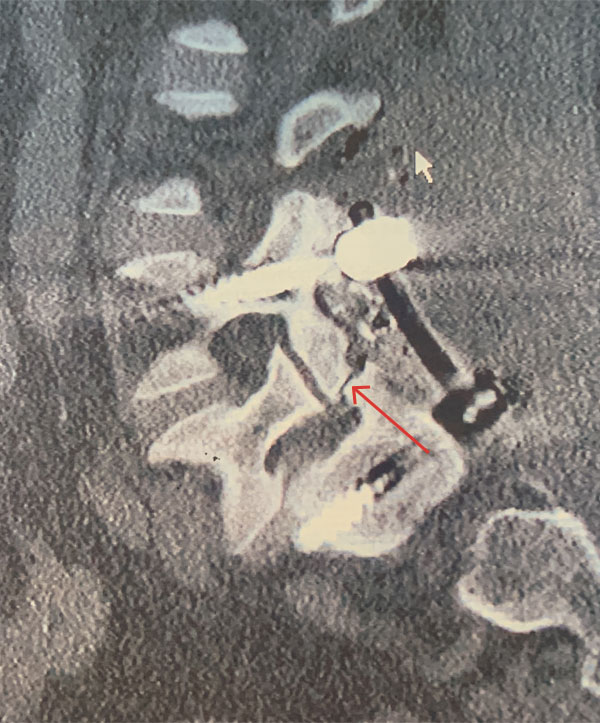
Figure 3 – Sagittal CT image showing post placement of posterior segmental fusion L4-S1 construct. Note pars deflect of L5 (arrow).
KEY LEARNING POINTS:
- Congenital, Dysplastic, or Isthmic Spondylolisthesis most commonly results from a fundamental defect in the posterior elements. It occurs most commonly at L5-S1 and is often associated with spina bifida occulta.
- Patients commonly have bilateral lytic separation of the pars interarticularis or spondylolysis which occurs in about 5 percent of the adult population with a 2:1 male to female ratio. This is in contrast to Degenerative Spondylolisthesis which occurs most commonly at L4-5, occurs as a result of degenerative changes in the disc and facet joints, allowing slippage, and is four times more common in females. Slippage occurs at L5-S1 in 90 percent of cases.
- Patients may also have elongation of the pars without lysis or dysplastic facet joints with abnormal sagittal orientation or development. Patients often have associated dysmorphic L5 vertebral bodies with secondary degeneration often at L4-5 as in this case.
- Congenital L5-S1 spondylolisthesis is the most common cause of low back pain in teens but patients may never manifest symptoms until adulthood or at all. Symptomatic patients typically will present with mechanical low back pain with or without radiculopathy. It is rare to develop a neurological deficit. Sometimes patients may only present with radiculopathy.
- Patients most commonly develop an L5 distribution radiculopathy as the nerve is affected at the level of the spondylolysis. Patients may also manifest abnormalities of gait or tight hamstrings. Most symptoms resolve with conservative management.
- Surgery is indicated in those patients who have pain unresolved with conservative therapy, progression of slip, or progressive neurological deficit. Patients who do require surgery typically undergo a laminectomy combined with instrumented fusion. Results do vary but overall patients experience approximately seventy-five percent relief of their symptoms.
CATEGORY: SPINE // LAMINECTOMY AND FUSION SOLVES DECADES OF BACK PAIN
Laminectomy and Fusion Solves Decades of Back Pain
A 44-year-old healthy female presented with over 20 years of chronic low back pain with associated intermittent right lower extremity pain that radiated to the foot.
She had failed all means of conservative management and presented for a surgical consultation. She was neurologically intact.