- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Unusual Indication for Carotid Stenting Over Endarterectomy
Non-Fusion Alternative for Treating Adjacent Segment Disease
April 14, 2022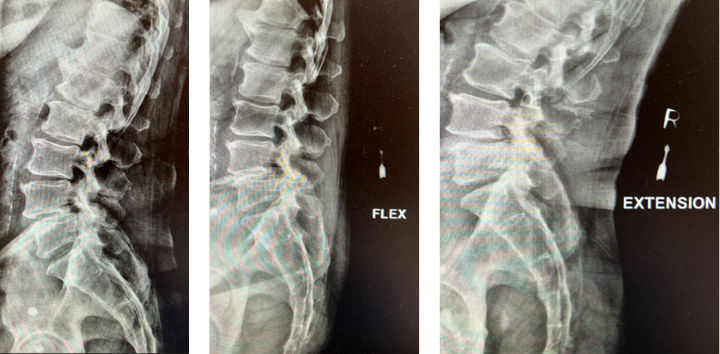
Treatment of Spondylolisthesis and Disc Herniation
May 13, 2022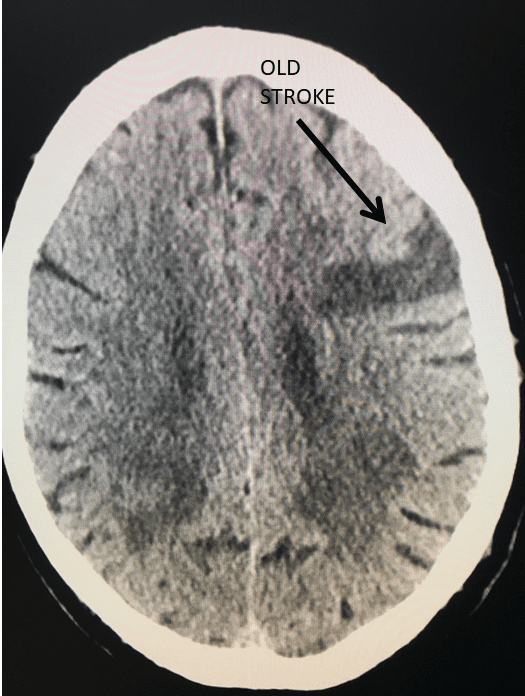
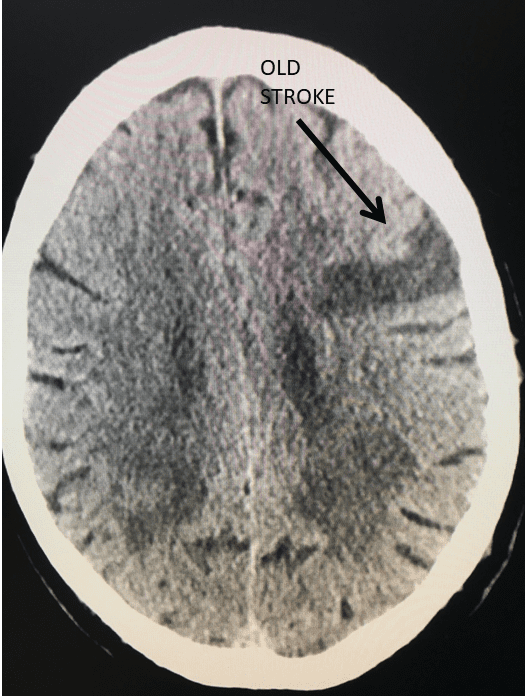
Figure 1.
This 77-year-old man with a history of stroke in 2013 presented to a small community hospital with aphasia upon awakening. Given the unclear timing of onset of his symptoms he was not deemed a candidate for intravenous thrombolytic. His NIHSS was 2 in the emergency room. He was admitted to the hospital where a CT (Figure 1) and CTA were performed showing a left frontal small infarct and severe extracranial carotid stenosis on the left. MRI could not be performed because of the patient’s pacemaker. Examination was significant for an awake gentleman with normal cranial nerve function and normal motor exam but significant expressive aphasia. Receptive aphasia was intact. He was placed on Aspirin.
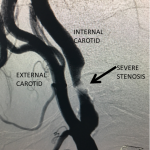
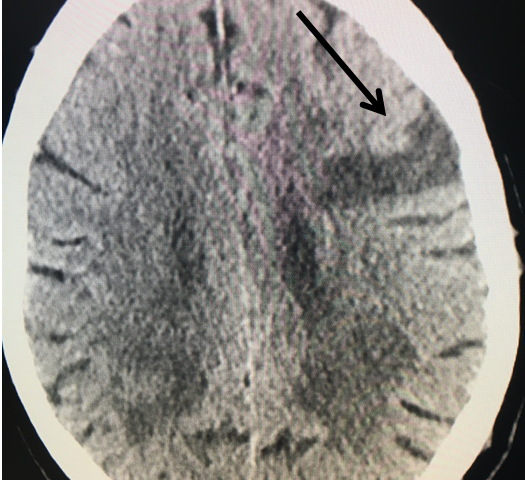
Figure 2.
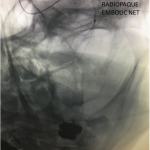
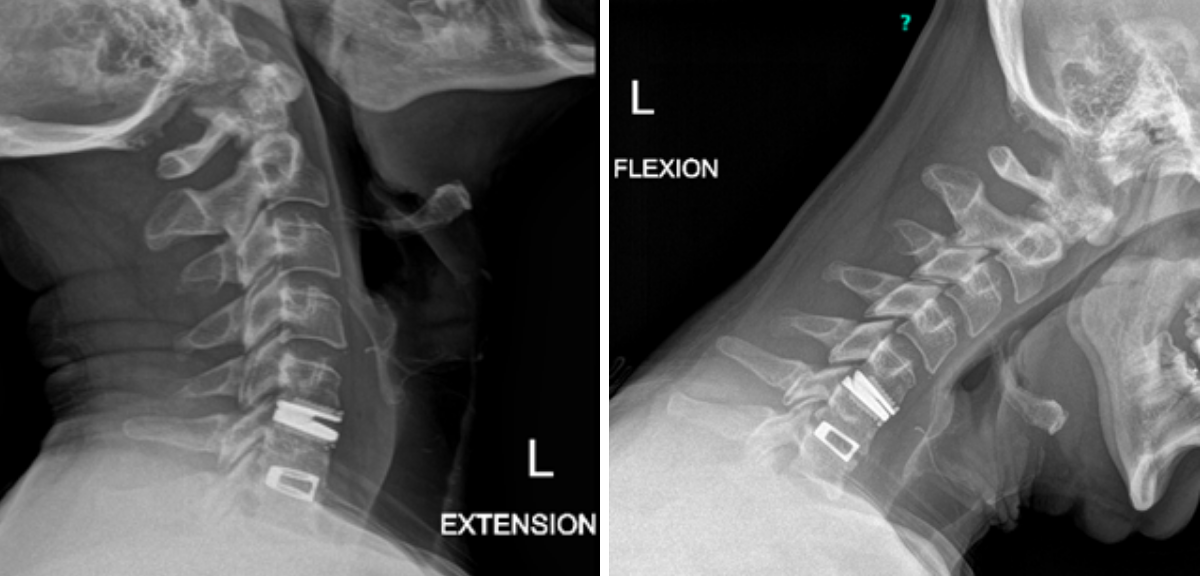
Figure 3.
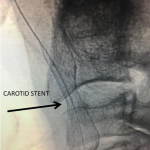
Figure 4.
The patient was brought to the operating room for a left carotid endarterectomy (CEA) after cardiologic evaluation deemed him a suitable candidate. After placing the patient under general anesthesia and positioning him with slight neck extension and head turned 30 degrees to the right a significant drop in somatosensory potentials of the left side of his body was noted. As this was the side ipsilateral to the carotid stenosis, an ischemic etiology was felt unlikely. Multiple attempts at repositioning failed to improve the potentials and the procedure was therefore aborted in favor of carotid angioplasty and stenting (CAS) under local anesthesia. He was transferred to our tertiary care regional facility for this procedure and loaded with Plavix in addition to his aspirin. Assays confirmed antiplatelet inhibition of both agents.
Catheter angiography prior to angioplasty revealed critical stenosis (Figure 2). Angioplasty was therefore performed under local anesthesia with an embolic protection device deployed to catch any dislodged debris (Figure 3). After angioplasty, a stent was opened across the lesion to maintain long-term patency (Figure 4). Post-stent angiography showed smooth dilatation of the lesion. The patient’s aphasia continued to improve at his 6-week follow-up visit and duplex revealed no significant stenosis through the stent.
DISCUSSION:
It is now considered Class I evidence (i.e. strongly in favor of benefit vs. risk) for patients experiencing non-disabling strokes or TIAs (including amaurosis fugax) who demonstrate greater than 70% carotid stenosis by non-invasive imaging to undergo carotid revascularization to reduce the chance of further strokes (2 year reduction of 26% recurrent stroke down to 9%).1-3 Revascularization is recommended by experienced surgeons only and includes carotid angioplasty and stenting (Level 2 evidence) or carotid endarterectomy (Level 1 evidence). American Heart Association guidelines recommend revascularization within 2 weeks preferably and no later than 6 months after the event in order to reap the stroke reduction with the accompanying risk of the procedure.3
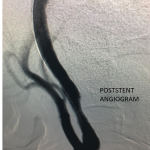
Figure 5.
The technical details of how I perform these procedures has been published previously and will not be recounted here.3 In general I recommend CEA for standard risk patients and reserve CAS for surgically high-risk patients as defined by the SAPPHIRE trial. These include patients with radiation stenosis, very high bifurcations, contralateral occlusion, severe pulmonary or cardiac disease or hostile surgical field as is the case with patients that have recurrent disease after prior CEA. Advanced age has been reconfigured as a surgical risk factor and generally I feel that CEA is safer in those older than 75 years, assuming they have no additional high-risk features. Based on the recent CREST trial, the patient described here was considered a good candidate for either procedure. Given the sensitivity of the monitoring potentials to positioning for CEA, this patient was treated with CAS successfully under local anesthesia. He was premedicated with Plavix and Aspirin and will continue on the Plavix for three months post-stenting and Aspirin indefinitely.
REFERENCES:
- Thomas G. Brott, M.D., Robert W. Hobson, II, M.D., George Howard, Dr.P.H., Gary S. Roubin, M.D., Ph.D.,Wayne M. Clark, M.D., William Brooks, M.D., Ariane Mackey, M.D., Michael D. Hill, M.D., Pierre P. Leimgruber, M.D., Alice J. Sheffet, Ph.D., Virginia J. Howard, Ph.D., Wesley S. Moore, M.D., Jenifer H. Voeks, Ph.D., L. Nelson Hopkins, M.D., Donald E. Cutlip, M.D., David J. Cohen, M.D., Jeffrey J. Popma, M.D., Robert D. Ferguson, M.D., Stanley N. Cohen, M.D., Joseph L. Blackshear, M.D., Frank L. Silver, M.D., J.P. Mohr, M.D., Brajesh K. Lal, M.D., and James F. Meschia, M.D.et al.,for the CREST Investigators* Stenting versus Endarterectomy for Treatment of Carotid-Artery Stenosis N Engl J Med 2010; 363:11-23
- North American Symptomatic Carotid Endarterectomy Trial Collaborators* Beneficial Effect of Carotid Endarterectomy in Symptomatic Patients with High-Grade Carotid Stenosis N Engl J Med 1991; 325:445-453
- Brisman, JL and Mayberg MR: Indications For Carotid Endarterectomy In Patients With Symptomatic Stenosis, in Stroke-Pathophysiology, Diagnosis and Management, Fifth Edition, 1398-1402 Elsevier Saunders, Philadelphia, PA, 2011
CATEGORY: ENDOVASCULAR // UNUSUAL INDICATION FOR CAROTID STENTING OVER ENDARTERECTOMY
Unusual Indication for Carotid Stenting Over Endarterectomy