- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Cysts
Sometimes It Is Obvious And Sometimes It Is Not
June 10, 2022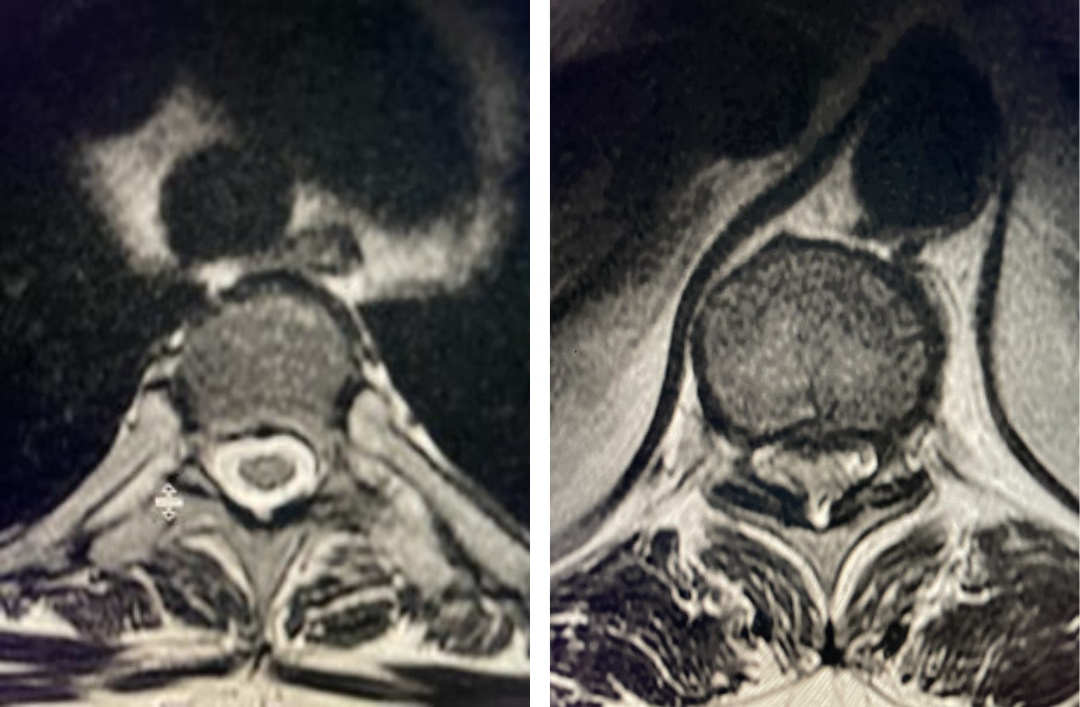
Thoracic Stenosis
July 22, 2022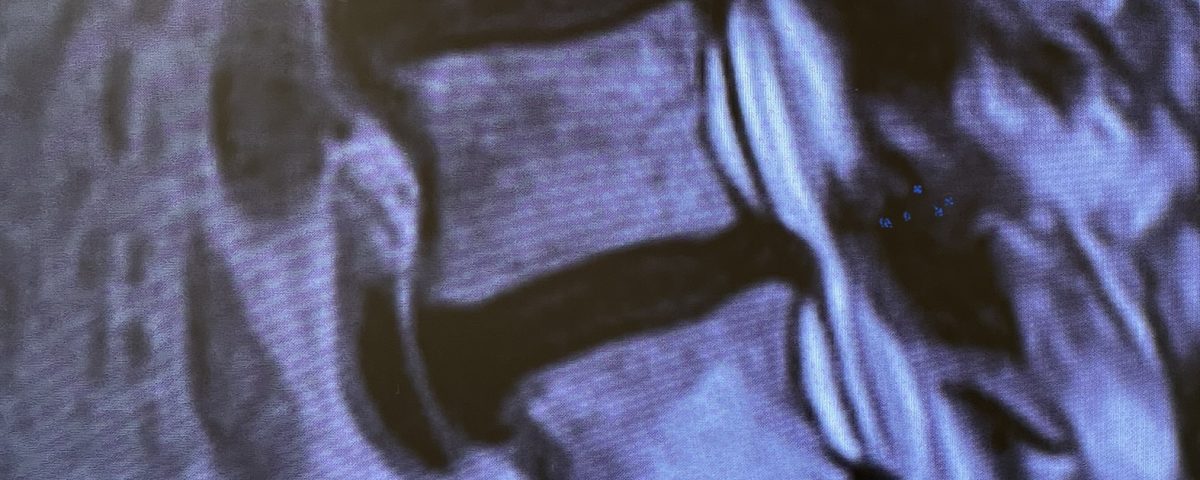
figure 2 cysts
People are obsessed with cysts! When you think about it, the body likes to form cysts. Why does this happen? Cysts can form just about anywhere in the body: the brain, ovaries, breast, kidney, joints, skin, and yes, the spine. The good thing about cysts is that they are usually benign. They are the resultant anatomical structure of an often-degenerative mechanism of the body. In the spine, patients will get into trouble by developing what is called a joint cyst or synovial cyst that are degenerative pathological extensions of the facet joint space. Perhaps secretions from the synovial lining are increased by the inflammatory process of arthritis; these joints are no different than a hip or knee joint. Maybe the loss of cartilage narrows the outflow of the synovial secretions in the joint space causing a cyst to form. The joint by not aligning properly will allow the synovium to find a path of least resistance to the epidural space. This synovium then forms a cyst outside of the joint space. This can result in compression of the descending nerve root in the subarticular space. Patients manifest radicular-type pain and are often associated with thickened ligamentous hypertrophy and manifest classic neurogenic claudication as well.
These cysts can often mimic the symptoms of a herniated disc; however, these cystic masses arise in the posterior compartment of the spinal canal. As in any usual presentation of lumbar stenosis or radiculopathy, we try to treat this conservatively with physical therapy, epidural injections, chiropractic care, and anti-inflammatories. Surgery is indicated for failure of conservative management with intractable pain or a progressive neurological deficit, which is a rarer presentation such as a foot drop. These cysts are not like a fluid-filled balloon which is what most people believe. Most patients ask, “why can’t you just aspirate the cyst?” The problem is that what you encounter intraoperatively is a cyst filled with thick gelatinous, necrotic material that is not very liquidy. Occasionally there is some fluid but in most cases the cyst cannot be percutaneously aspirated. These patients require direct visualization to remove the cyst as they are often very adherent to the dura. It is vital to find the root that is being compressed so one can develop a plane of separation of the cyst from the root. In most cases the majority of the cyst wall can be dissected and removed, and the internal material can be evacuated. By just removing it piecemeal you get the majority of the cyst and remove the mass effect. In many cases part of the wall can be so adherent it seems to meld with the dura. There is no reason to attempt to remove the entire wall as you risk a dural tear and CSF leak. The most important goal is to DECOMPRESS the nerve root; it is ok to leave part of the cyst attached to the dura as long as the mass effect is gone. After the surgery the first thing that patients and patients’ family members ask is “did you get the cyst?” What they need to ask is if the nerve root is well decompressed? In almost all cases the cyst is gone, but at this point in my career I know that is not what is most important.
Case Study
This 63-year-old female presents with nine months of low back pain and pain radiating to the lower extremities with the left leg worse than the right. The patient complained of numbness and tingling as well. The pain was exacerbated by standing, walking, and coughing. An MRI demonstrated severe lumbar stenosis L3-L5 with a superimposed left L3-4 synovial cyst (Fig 1).
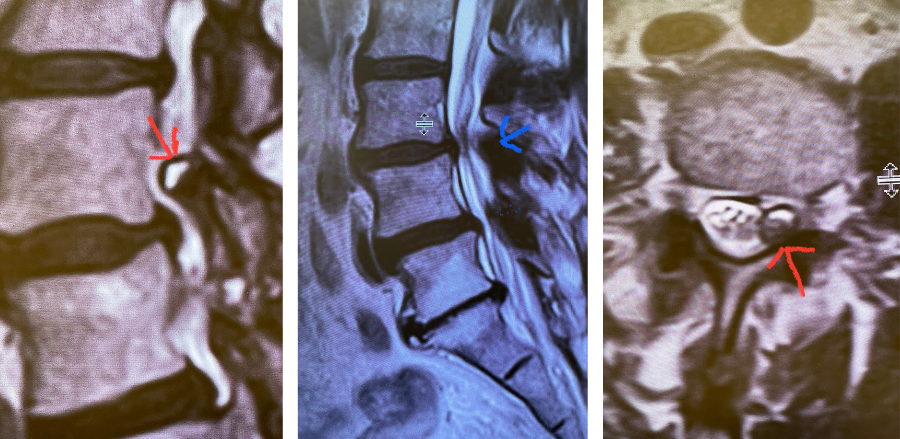
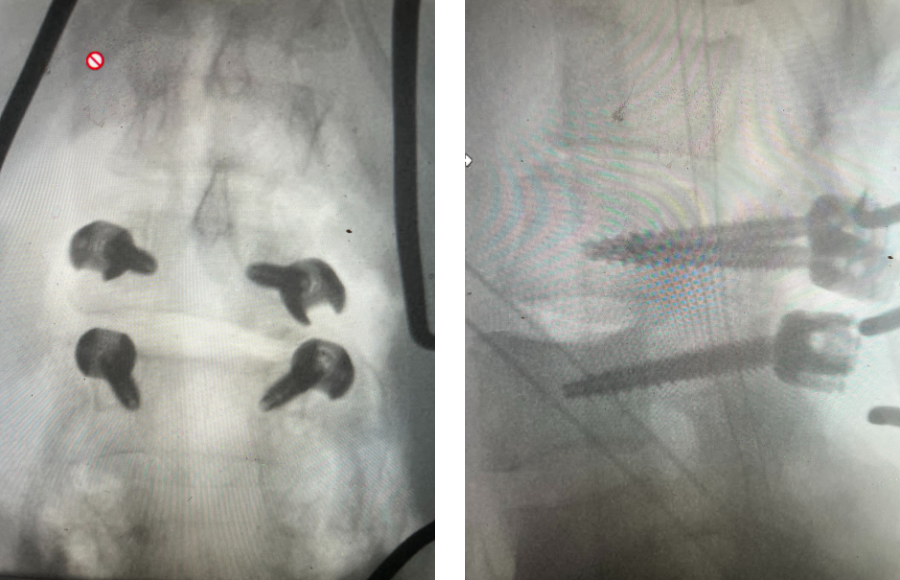
Fig 1: Sagittal and axial T2-weighted MRI images demonstrating a large superiority-oriented synovial cyst (red arrow) at L4-5. The cyst is below the exiting L4 nerve root and hence compresses the descending L5 root. Note the additional thickened ligamentum flavum and slight spondylolistheses at L3-4 and L4-5 (blue arrow).
The patient also had a slight spondylolisthesis at L3-4 and L4-5. The patient failed all means of conservative management including medications, physical therapy, and epidural injections. The patient elected to proceed with a decompressive laminectomy and in-situ fusion. During the procedure we encountered a thick-walled cyst that melded with the dura. We first found the descending left L4 nerve root and separated the cyst and proceeded to in essence bite away the cyst with an instrument. We decompressed the L4 nerve root as it entered its foramina by removing the majority of the cyst wall. There was thick gray gelatinous material within the cyst. Part of the cyst wall seemed to be continuous with the dura and left it alone as it caused no pressure on the root. After our decompression we decided to perform an in-situ fusion as we had relative preservation of the joint complexes. Post operatively, she had an uneventful course with significant relief of her leg pain.


