June 25, 2024
- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
Studies
June 19, 2024
REVISION SURGERY TREATS INTRACTABLE NECK PAIN & CERVICAL DEFORMITY Clinical Presentation The patient is a 61-year-old female with a history of rheumatoid arthritis. She is 2-1/2-years […]
May 8, 2024
July 26, 2023
“Here’s What Came in Today” by Dr. William Sonstein I specialize in and am very familiar with patients who have osteoporosis and require spinal surgery for […]
July 24, 2023
I specialize in and am very familiar with patients who have osteoporosis and require spinal surgery for degenerative lumbar disease. I am particularly interested in treating […]
August 29, 2022
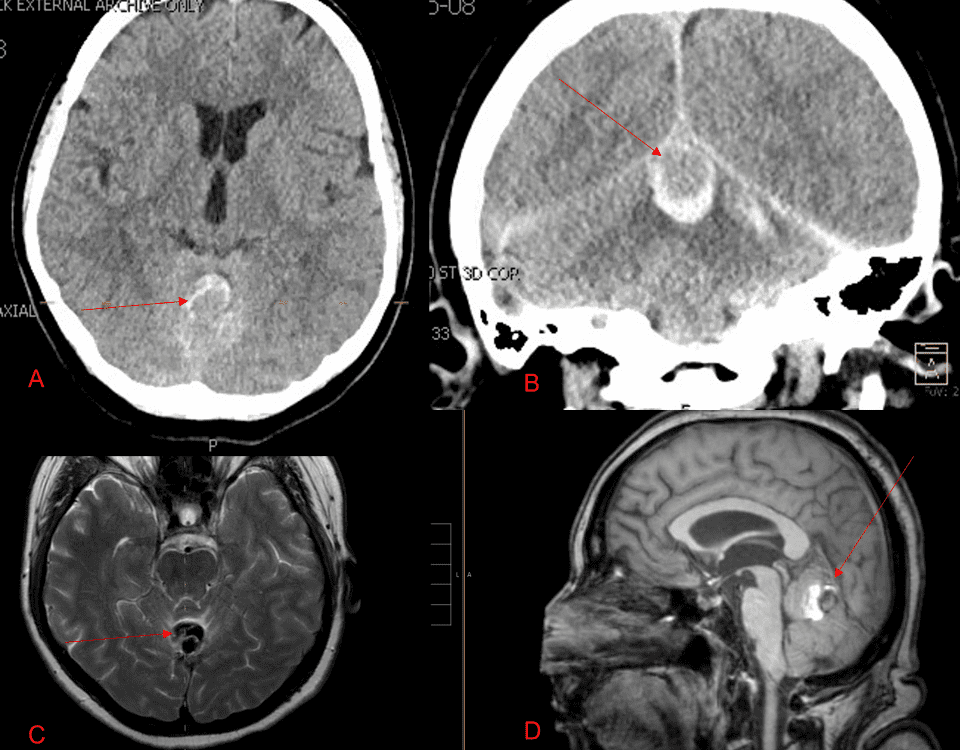
A 55-year-old woman presented with acute onset of severe headache, and possible witnessed seizure. Imaging confirmed intraventricular hemorrhage primarily focused within the fourth ventricle with diffuse […]
July 22, 2022
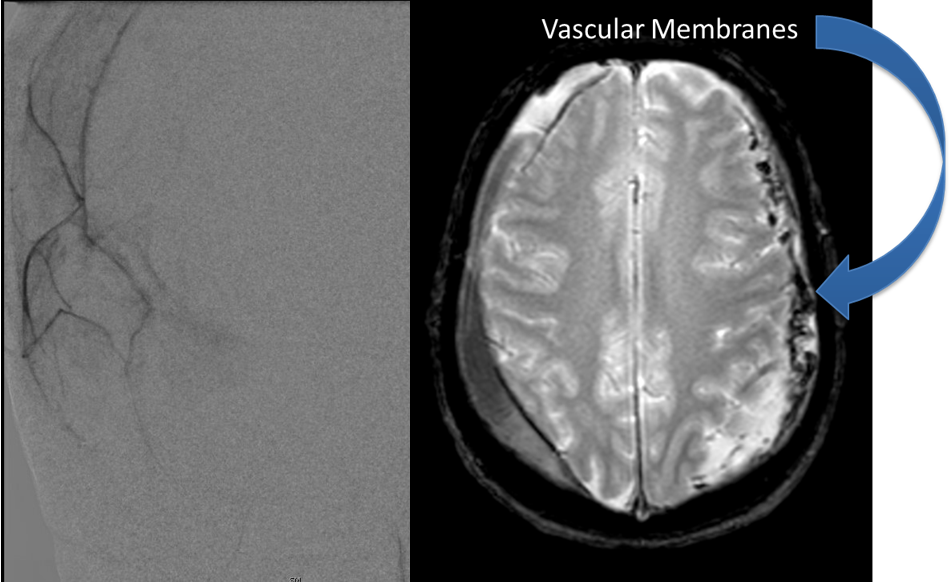
Case Presentation: A woman in her 80s developed mild dizziness and headache following incidental trauma working in her garage one day. She presented several weeks later […]
July 21, 2022
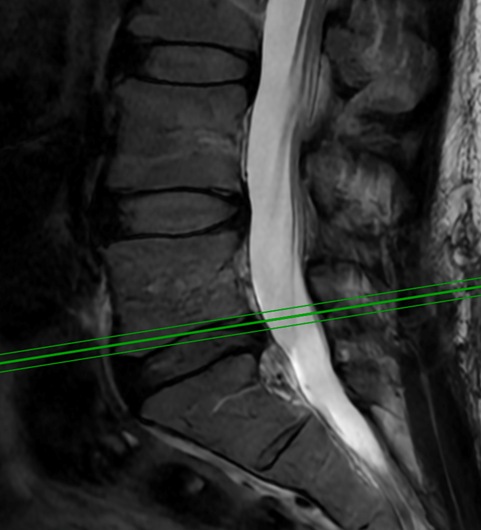
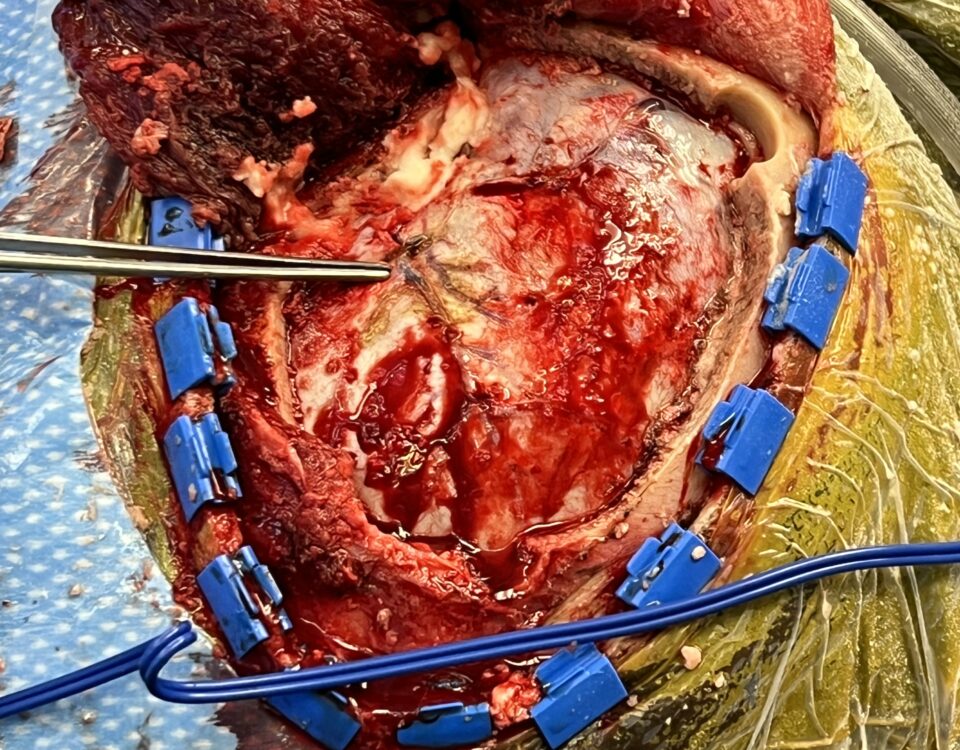
This 62-year-old female presents with chronic intractable low back pain with radiation down the front of her thighs. The patient had had two prior fusion surgeries: […]
July 1, 2022
The patient is an 83-year-old man who has a history of hypertension and prior strokes who presented with a brief episode of left arm greater than […]