- PATIENT FORMS | REQUEST A CONSULTATION | CONTACT US
- 1-844-NSPC-DOC
NSPC Neurosurgeon Dr. Michael Brisman Authors Brain Surgery TextbookClick Here To Learn More
Dr. William Sonstein Co-Authors Article on Cerebrospinal Fluid Diagnostic Test Strip for CNS' PublicationClick Here To Learn More
Studies
July 26, 2023
July 26, 2023
“Here’s What Came in Today” by Dr. William Sonstein I specialize in and am very familiar with patients who have osteoporosis and require spinal surgery for […]
July 24, 2023
July 24, 2023
I specialize in and am very familiar with patients who have osteoporosis and require spinal surgery for degenerative lumbar disease. I am particularly interested in treating […]
August 29, 2022
August 29, 2022
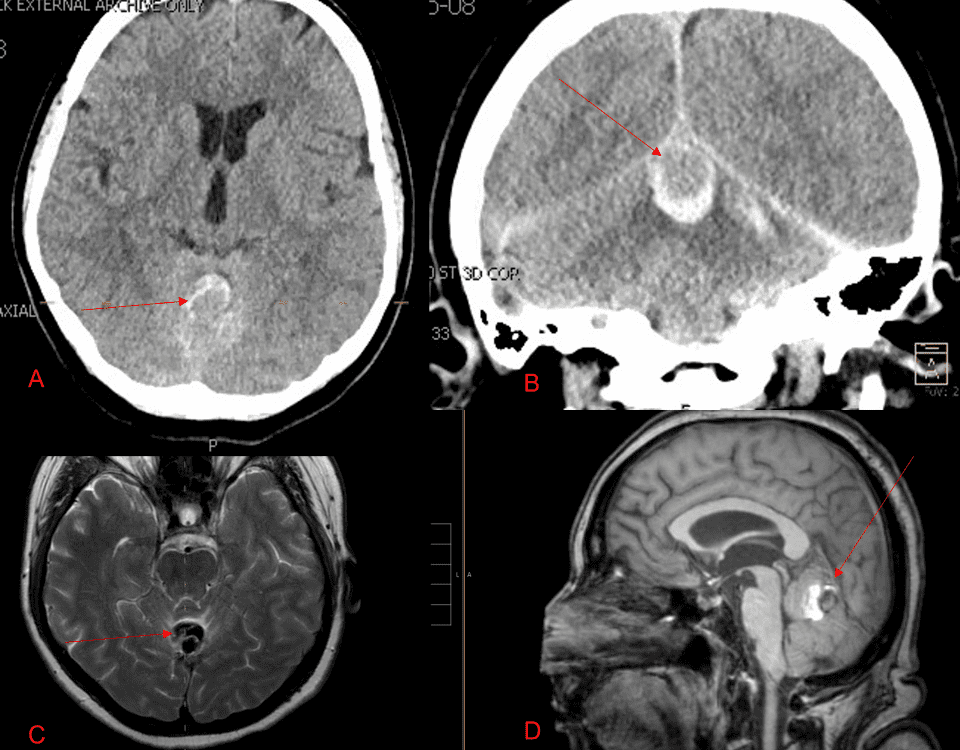
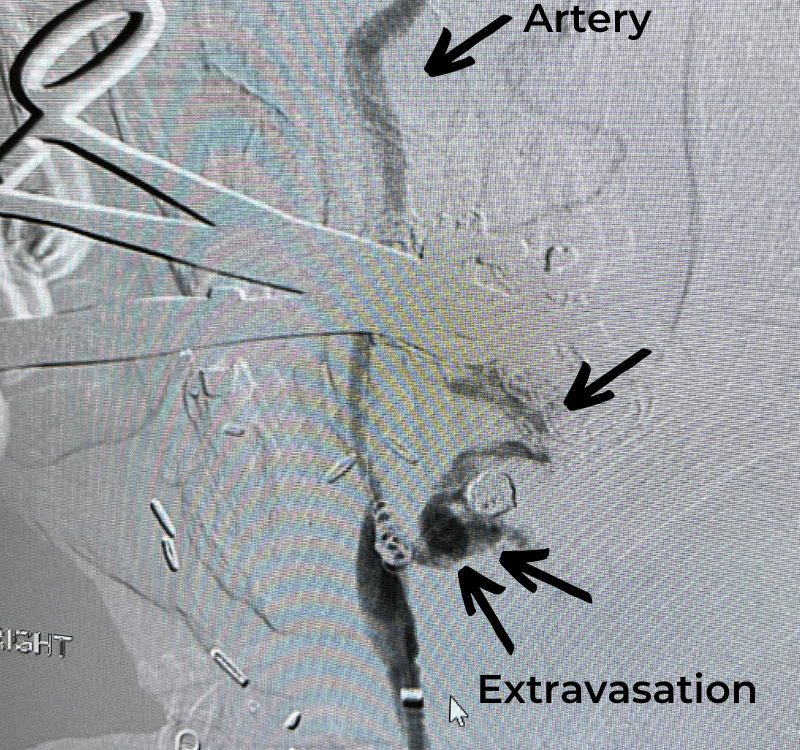
A 55-year-old woman presented with acute onset of severe headache, and possible witnessed seizure. Imaging confirmed intraventricular hemorrhage primarily focused within the fourth ventricle with diffuse […]
July 22, 2022
July 22, 2022
Case Presentation: A woman in her 80s developed mild dizziness and headache following incidental trauma working in her garage one day. She presented several weeks later […]
July 21, 2022
July 21, 2022
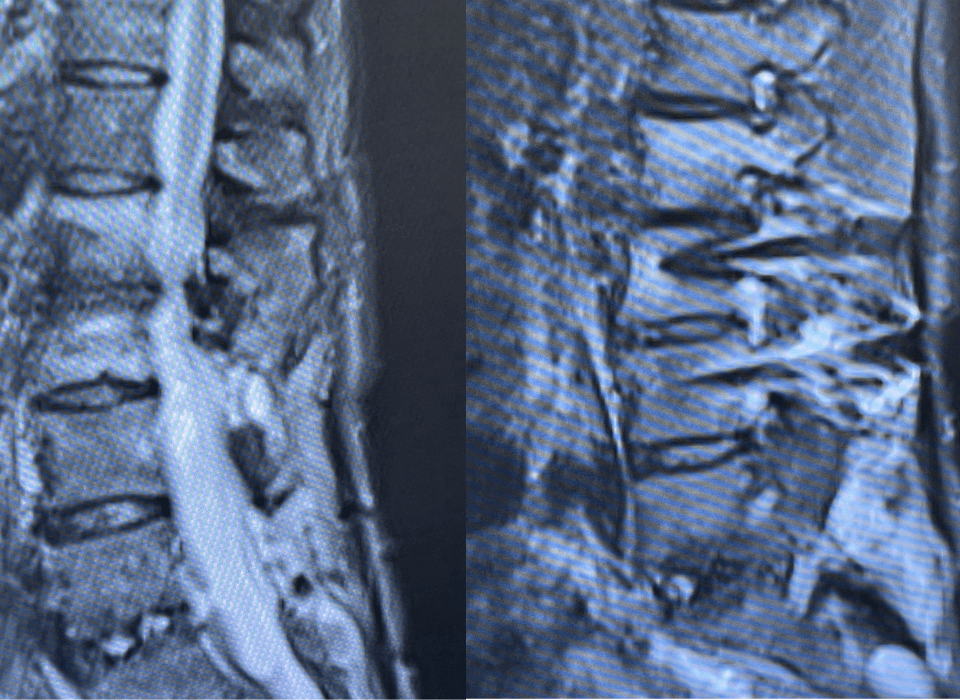
This 62-year-old female presents with chronic intractable low back pain with radiation down the front of her thighs. The patient had had two prior fusion surgeries: […]
July 1, 2022
July 1, 2022
The patient is an 83-year-old man who has a history of hypertension and prior strokes who presented with a brief episode of left arm greater than […]
June 27, 2022
June 27, 2022
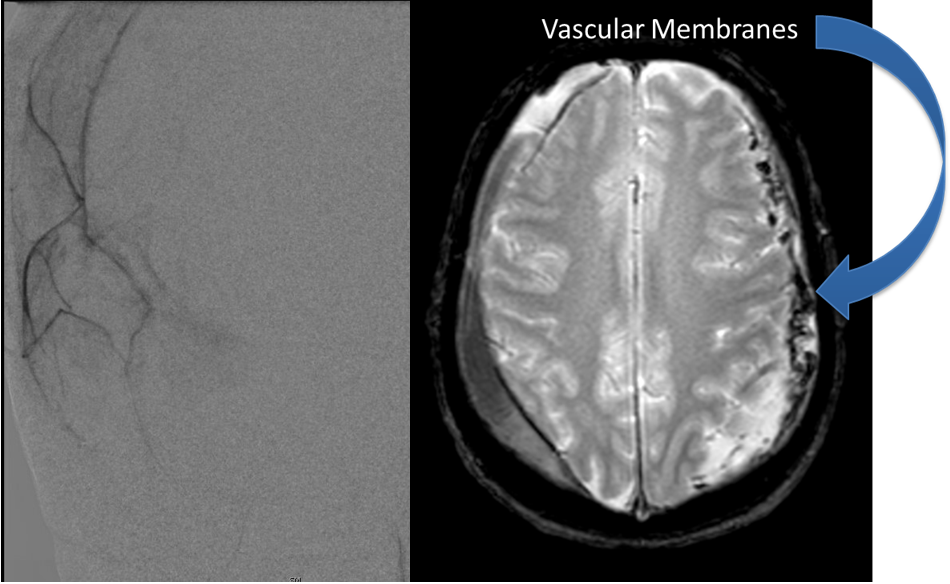
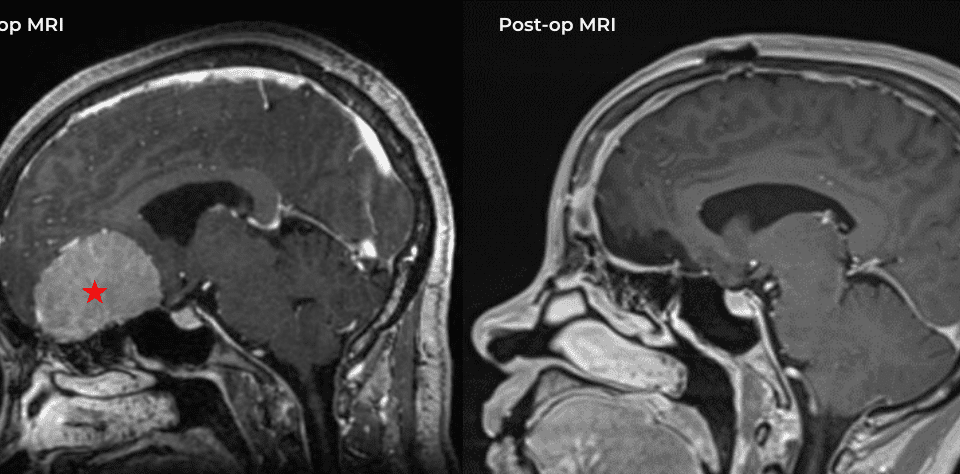
This is a 49-year-old otherwise healthy female who presented with bifrontal and retro-orbital headaches, behavioral changes, and forgetfulness. Symptoms have been progressively worsening over the past […]
June 16, 2022
June 16, 2022
The patient is a 57-year-old woman with a long history of tonsillar cancer, treated in the past with multiple surgical procedures including right-sided mandibular surgery and […]
June 9, 2022
June 9, 2022
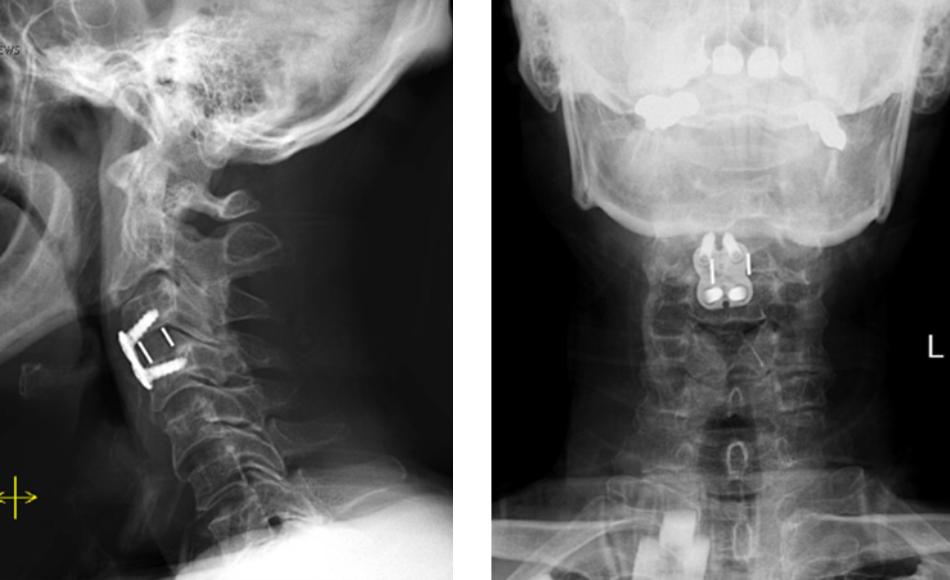
This patient is a 65-year-old man who presented to the ER after a fall from a horse. He was unable to move his arms but had […]